
Mga EHR at EMR: Ang Backbone ng Digital Health Records
11 Nov, 2023
 Healthtrip Team
Healthtrip TeamSa mabilis na umuusbong na landscape ng pangangalagang pangkalusugan ngayon, ang pag-digitize ng mga rekord ng kalusugan ay naging pundasyon ng mga modernong sistema ng pangangalagang pangkalusugan.. Ang Electronic Health Records (EHRs) at Electronic Medical Records (EMRs) ay ang mga puwersang nagtutulak sa likod ng pagbabagong ito, na nag-aalok ng komprehensibo at magkakaugnay na diskarte sa pamamahala ng impormasyon ng pasyente. Ang blog na ito ay susuriin sa mga intricacy ng EHR at EMR, paggalugad ng kanilang malalim na kabuluhan at malayong epekto sa industriya ng pangangalagang pangkalusugan.
Baguhin ang iyong kagandahan, Palakasin ang Iyong Kumpiyansa
Maghanap ng tamang kosmetiko pamamaraan para sa iyong mga pangangailangan.

Dalubhasa kami sa isang malawak na hanay ng mga cosmetic procedure

Mga EHR at EMR
A. Electronic Health Records (EHRs):):
1. Electronic Health Records (EHRs)ay ang mga digital na katapat ng tradisyonal na papel na nakabatay sa mga tala ng pasyente. Ang mga ito ay idinisenyo upang magbigay ng isang holistic na pagtingin sa kasaysayan ng medikal ng isang pasyente at mga pakikipag-ugnayan sa pangangalagang pangkalusugan sa iba't ibang mga provider at organisasyon ng pangangalagang pangkalusugan. Narito ang isang breakdown ng mga pangunahing bahagi at functionality ng EHRs:
2. Komprehensibong Impormasyon ng Pasyente: Ang EHRS ay nag -iimbak ng isang malawak na hanay ng data ng pasyente, kabilang ang mga personal na demograpiko, kasaysayan ng medikal, kasalukuyan at nakaraang mga diagnosis, gamot, alerdyi, mga tala sa pagbabakuna, at kasaysayan ng medikal na pamilya. Ang komprehensibong profile ng pasyente ay tumutulong sa mga nagbibigay ng pangangalaga sa kalusugan na gumawa ng mga kaalamang desisyon.
3. Accessibility: Ang isa sa mga pangunahing bentahe ng EHR ay ang kanilang pag -access. Ang mga awtorisadong propesyonal sa pangangalagang pangkalusugan ay maaaring ma -access ang mga EHR nang ligtas mula sa iba't ibang mga lokasyon, kabilang ang mga ospital, klinika, at kahit na malayo, salamat sa pag -secure ng mga kredensyal sa pag -login at advanced na pag -encrypt.
4. Interoperability: Ang mga EHR ay idinisenyo upang maging interoperable, nangangahulugang maaari silang makipag -usap at makipagpalitan ng data sa iba't ibang mga sistema ng pangangalaga sa kalusugan at tagapagkaloob. Tinitiyak ng interoperability na ito ang pagbabahagi ng seamless data sa mga organisasyon ng pangangalagang pangkalusugan, na nagtataguyod ng mas mahusay na koordinasyon ng pangangalaga at mga resulta ng pasyente.
5. Suporta sa Desisyon ng Klinikal: Ang mga EHR ay madalas na nagtatampok ng mga tool sa suporta sa desisyon ng klinikal na tumutulong sa mga nagbibigay ng pangangalagang pangkalusugan sa paggawa ng mga kaalamang desisyon. Ang mga tool na ito ay maaaring magbigay ng mga alerto para sa mga potensyal na pakikipag-ugnayan sa gamot, paalalahanan ang mga tagapagbigay ng inirekumendang pag-screen, at mag-alok ng mga rekomendasyong paggamot na batay sa ebidensya.
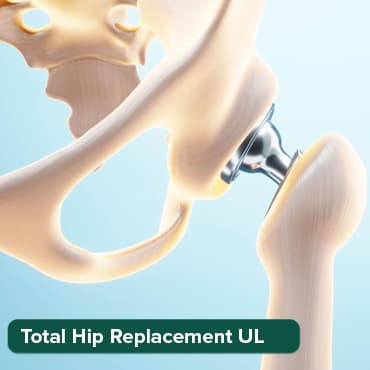
Pinakatanyag na mga pamamaraan sa India
Kabuuang Pagpapalit
Hanggang 80% diskwento
90% Na-rate
Kasiya-siya
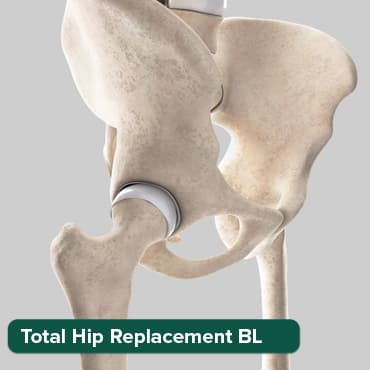
Kabuuang Pagpapalit
Hanggang 80% diskwento
90% Na-rate
Kasiya-siya
Kabuuang Pagpapalit
Hanggang 80% diskwento
90% Na-rate
Kasiya-siya

ANGIOGRAM
Hanggang 80% diskwento
90% Na-rate
Kasiya-siya

Pagsara ng ASD
Hanggang 80% diskwento
90% Na-rate
Kasiya-siya

6. Imaging at Mga Resulta ng Pagsubok: Ang mga EHR ay maaaring mag-imbak ng mga larawan ng radiology, mga resulta ng lab, at iba pang data ng diagnostic, na ginagawang mas madali para sa mga tagapagbigay ng pangangalagang pangkalusugan na ma-access at masuri ang mga kritikal na piraso ng impormasyong ito.
7. Data ng Pagsingil at Administratibo: Maaaring kabilang sa mga EHR ang data ng pagsingil at administratibo, pagpapasimple sa pamamahala ng mga pananalapi sa pangangalagang pangkalusugan at pagbabawas ng administratibong overhead para sa mga organisasyon ng pangangalagang pangkalusugan.
B. Mga Electronic Medical Records (EMRs):
Ang Electronic Medical Records (EMRs) ay nagbabahagi ng maraming pagkakatulad sa mga EHR ngunit karaniwang limitado ang saklaw sa isang partikular na pasilidad o kasanayan sa pangangalagang pangkalusugan.. Narito ang isang mas malapit na pagtingin sa mga EMR:
1. Nakasentro sa Pasilidad: Pangunahing ginagamit ang mga EMR sa loob ng isang pasilidad o kasanayan sa pangangalagang pangkalusugan, tulad ng isang ospital, klinika, o pribadong kasanayan. Ang mga ito ay dinisenyo upang makuha at pamahalaan ang impormasyon ng pasyente na nabuo sa loob ng tiyak na samahan.
2. Pangangalagang Nakasentro sa Pasyente: Ang mga EMR ay nakatulong sa pagbibigay ng pangangalagang nakasentro sa pasyente sa loob ng mga limitasyon ng isang partikular na setting ng pangangalagang pangkalusugan. Binibigyang-daan nila ang mga tagapagbigay ng pangangalagang pangkalusugan sa loob ng organisasyon na ma-access ang napapanahong impormasyon ng pasyente, i-streamline ang mga daloy ng trabaho, at tiyakin ang pagpapatuloy ng pangangalaga.
3. Imbakan ng data at pagkuha: Ang mga EMR ay nag-iimbak ng mahahalagang data ng pasyente, kabilang ang mga medikal na kasaysayan, diagnosis, paggamot, at mga resulta ng pagsusuri. Pinapayagan nila ang mahusay na pagkuha ng impormasyong ito sa panahon ng mga engkwentro ng pasyente, na binabawasan ang pangangailangan para sa mga rekord ng papel at manu-manong pagpasok ng data.
4. Pagsasama: Bagama't ang mga EMR ay maaaring walang parehong antas ng interoperability gaya ng mga EHR, maaari pa rin silang magsama sa iba pang mga system sa loob ng parehong pasilidad ng pangangalagang pangkalusugan, gaya ng mga laboratoryo system at software sa pagsingil.
Ang Kahalagahan ng mga EHR at EMR:
1. Pinahusay na Pangangalaga sa Pasyente:
Malaki ang kontribusyon ng mga EHR at EMR sa pagpapabuti ng pangangalaga sa pasyente sa iba't ibang paraan:
1. Komprehensibong Impormasyon ng Pasyente: Sa pamamagitan ng access sa kumpletong medikal na kasaysayan ng isang pasyente, ang mga propesyonal sa pangangalagang pangkalusugan ay maaaring gumawa ng mas tumpak na mga diagnosis at gumawa ng mga iniakmang plano sa paggamot. Kasama sa komprehensibong pananaw na ito ang mga nakaraang sakit, gamot, allergy, at iba pang kritikal na data na nagpapaalam sa mga desisyon sa pangangalagang pangkalusugan.
2. Suporta sa Klinikal na Desisyon: Nag-aalok ang mga EHR ng built-in na mga tool sa suporta sa klinikal na desisyon na nagbibigay ng mga real-time na alerto at rekomendasyon. Halimbawa, kung ang isang doktor ay nagrereseta ng isang gamot na maaaring makipag-ugnayan sa mga kasalukuyang gamot o allergy ng isang pasyente, ang system ay maaaring mag-isyu ng isang alerto, na pumipigil sa potensyal na pinsala.
3. Malayong Pag-access: Pinapagana ng EHR ang mga nagbibigay ng pangangalagang pangkalusugan na ma-access ang impormasyon ng pasyente nang malayuan, na lalo na mahalaga para sa pag-aalaga ng telemedicine at pagkatapos ng oras. Tinitiyak ng accessibility na ito ang patuloy na pangangalaga at napapanahong pagtugon sa mga pangangailangan ng pasyente.
4. Koordinasyon ng Pangangalaga: Pinapadali ng mga EHR ang koordinasyon ng pangangalaga sa iba't ibang mga espesyalista at mga setting ng pangangalagang pangkalusugan. Kapag maraming provider ang may access sa parehong mga talaan, maaari silang makipagtulungan nang mas epektibo, binabawasan ang redundancy at tinitiyak na ang plano sa pangangalaga ng pasyente ay magkakaugnay at may kaalamang mabuti.
2. Streamline na daloy ng trabaho:
Ang paglipat mula sa mga talaang nakabatay sa papel patungo sa mga digital na talaan ng kalusugan ay may malaking epekto sa kahusayan ng daloy ng trabaho::
1. Nabawasan ang pasanin ng administratibo: Tinatanggal ng mga EHR ang pangangailangan para sa manu-manong gawaing papel, na binabawasan ang administratibong overhead. Pinapayagan nito ang mga kawani ng pangangalagang pangkalusugan na mag -focus nang higit pa sa pangangalaga ng pasyente at mas kaunti sa mga gawaing pang -administratibo tulad ng pag -file at pagpasok ng data.
2. Mas Mabilis na Pag-access sa Impormasyon: Maaaring ma-access agad ng mga nagbibigay ng pangangalaga sa kalusugan ang mga tala ng pasyente, pag-iwas sa mga paghahanap sa oras para sa mga file ng papel. Ang mabilis na pag-access sa impormasyon ay nagpapabilis sa mga nakatagpo ng pasyente at pinapabuti ang pangkalahatang karanasan ng pasyente.
3. Automation: Ang mga EHR ay madalas na kasama ang mga awtomatikong tampok tulad ng pag -iskedyul ng appointment, mga kahilingan sa pag -renew ng reseta, at mga proseso ng pagsingil. Ang mga tampok na automation na ito ay nag -streamline ng mga proseso ng administratibo at bawasan ang mga error.
3. Pinahusay na Komunikasyon:
Ang epektibong komunikasyon ay mahalaga sa pangangalagang pangkalusugan, at pinapadali ng mga EHR ang tuluy-tuloy na pagpapalitan ng impormasyon:
1. Komunikasyon ng Inter-Provider: Pinapagana ng EHR ang iba't ibang mga propesyonal sa pangangalagang pangkalusugan na makipag -usap at makipagtulungan nang mas epektibo. Ang mga espesyalista, pangunahing manggagamot sa pangangalaga, nars, at iba pang mga miyembro ng koponan ay maaaring ma-access ang parehong mga talaan ng pasyente, tinitiyak na mayroon silang pinaka-napapanahon na impormasyon para sa kaalamang pagpapasya.
2. Pakikipag -ugnayan sa pasyente: Ang mga EHR ay madalas na may mga portal ng pasyente na nagpapahintulot sa mga pasyente na ma -access ang kanilang sariling mga tala sa kalusugan at makipag -usap sa kanilang mga nagbibigay ng pangangalaga sa kalusugan. Pinapabuti nito ang pakikipag-ugnayan ng pasyente at binibigyang kapangyarihan ang mga indibidwal na aktibong lumahok sa kanilang pangangalaga.
4. Data Analytics at Pananaliksik:
Ang mga EHR at EMR ay nagsisilbing mahalagang mapagkukunan ng data para sa pananaliksik at pagsusuri:
1. Pamamahala sa Kalusugan ng Populasyon: Maaaring gamitin ng mga organisasyon ng pangangalagang pangkalusugan ang data ng EHR upang matukoy ang mga uso at pattern sa mga populasyon ng pasyente. Ang impormasyong ito ay nakakatulong sa pamamahala ng mga inisyatibo sa kalusugan ng publiko at mga diskarte sa pangangalaga sa pag -aalaga.
2. Klinikal na pananaliksik: Maaaring ma-access ng mga mananaliksik ang data ng hindi natukoy na pasyente mula sa mga EHR upang magsagawa ng mga klinikal na pagsubok at pag-aaral. Ang data na ito ay maaaring humantong sa mga pagsulong sa kaalaman sa medikal, pag -unlad ng gamot, at mga protocol ng paggamot.
3. Pagpapabuti ng Kalidad: Ang mga EHR ay nagbibigay ng mga pananaw sa kalidad ng pangangalaga na naihatid sa loob ng mga organisasyong pangkalusugan. Sa pamamagitan ng pagsusuri sa data ng EHR, matutukoy ng mga institusyon ang mga lugar para sa pagpapabuti at ipatupad ang mga kasanayang nakabatay sa ebidensya upang mapahusay ang mga resulta ng pasyente.
Sa konklusyon, ang mga EHR at EMR ay hindi lamang nagpapabuti sa pangangalaga sa pasyente ngunit mayroon ding malalayong benepisyo, kabilang ang mga streamline na daloy ng trabaho, pinahusay na komunikasyon, at suporta para sa data-driven na pananaliksik at pagpapabuti ng kalidad ng pangangalaga sa kalusugan. Ang kanilang papel bilang mga tool na pang -pundasyon sa modernong pangangalaga sa kalusugan ay patuloy na nagbabago at nagtutulak ng mga pagpapabuti sa paghahatid ng kalusugan.
Mga Hamon at Alalahanin:
Habang ang mga EHR at EMR ay nag-aalok ng maraming benepisyo, mayroon din silang ilang hamon at alalahanin:
1. Seguridad ng Data::
Ang seguridad ng data ay pinakamahalaga sa pangangalagang pangkalusugan, dahil sa pagiging sensitibo ng impormasyon ng pasyente. Kasama sa mga hamon at alalahanin sa lugar na ito:
1. Mga Paglabag sa Data: Ang sektor ng pangangalagang pangkalusugan ay isang pangunahing target para sa cyberattacks, dahil ang mga rekord ng pasyente ay naglalaman ng mahalagang personal at pinansyal na impormasyon. Ang mga paglabag sa data ay maaaring magresulta sa makabuluhang pinsala sa mga pasyente at pinsala sa reputasyon ng mga organisasyong pangkalusugan.
2. Hindi awtorisadong Pag-access: Ang pagpigil sa hindi awtorisadong pag-access sa mga rekord ng pasyente ay mahalaga. Ang malakas na kontrol sa pag-access, secure na paraan ng pagpapatotoo, at audit trail ay kinakailangan para matiyak na ang mga awtorisadong tauhan lang ang makakatingin at makakapagbago ng data ng pasyente.
3. Pag-encrypt: Ang pag-encrypt ng data ay mahalaga para sa pagprotekta sa data ng pasyente kapwa sa pahinga at sa panahon ng paghahatid. Tinitiyak nito na kahit na mangyari ang hindi awtorisadong pag-access, ang data ay nananatiling hindi maintindihan nang walang wastong mga decryption key.
4. Mga Protokol ng Cybersecurity: Ang mga organisasyon ng pangangalagang pangkalusugan ay dapat magpatupad ng matatag na mga protocol sa cybersecurity upang ipagtanggol laban sa malware, ransomware, at iba pang banta sa cyber. Ang mga regular na pag-audit at pag-update sa seguridad ay mahalaga upang manatiling nangunguna sa mga umuusbong na banta.
2. Interoperability: Interoperability::
Ang mga hamon sa interoperability ay nauugnay sa kakayahan ng iba't ibang EHR at EMR system na gumana nang walang putol:
1. Mga Pamantayan sa Data: Ang mga system ng pangangalaga sa kalusugan ng IT ay madalas na gumagamit ng iba't ibang mga format at pamantayan ng data, na ginagawang mahirap na makipagpalitan ng impormasyon. Ang mga pagsusumikap sa standardisasyon, gaya ng HL7 at FHIR (Fast Healthcare Interoperability Resources), ay naglalayong tugunan ang isyung ito sa pamamagitan ng paglikha ng mga karaniwang pamantayan sa pagpapalitan ng data.
2. Teknikal na Pagsasama: Ang pagsasama ng mga EHR at EMR sa iba pang mga sistema ng pangangalagang pangkalusugan, tulad ng mga sistema ng laboratoryo o mga sistema ng parmasya, ay maaaring maging kumplikado. Ang mga isyu sa pagiging tugma at magkakaibang mga pagtutukoy sa teknikal ay maaaring hadlangan ang interoperability.
3. Pagmamapa ng Data at Pagsasalin: Ang pagmamapa ng data at pagsasalin ay kinakailangan upang matiyak na ang impormasyon mula sa isang sistema ay mauunawaan at magagamit ng iba. Nangangailangan ito ng standardized na proseso ng pagmamapa ng data at maingat na pangangasiwa ng semantic interoperability.
4. Pagtutugma ng Pasyente: Ang tumpak na pagtutugma ng pasyente ay mahalaga upang maiwasan ang mga pagkakamali sa pangangalaga sa kalusugan. Ang pagtiyak na ang mga tala ay tama na naitugma sa tamang pasyente, lalo na sa mga multi-system na kapaligiran, ay isang makabuluhang hamon.
3. Pagsasanay sa gumagamit:
Ang epektibong paggamit ng mga EHR at EMR ay nakasalalay sa kahusayan ng mga propesyonal sa pangangalagang pangkalusugan:
1. Programa para sa pagsasanay: Ang mga organisasyon ng pangangalagang pangkalusugan ay dapat magbigay ng komprehensibong mga programa sa pagsasanay upang maging pamilyar ang mga kawani sa EHR o EMR system. Ang pagsasanay na ito ay dapat masakop ang nabigasyon ng system, pagpasok ng data, at pinakamahusay na kasanayan para sa dokumentasyon.
2. Patuloy na Edukasyon: Ang mga EHR at EMR ay patuloy na umuunlad, at ang mga propesyonal sa pangangalagang pangkalusugan ay nangangailangan ng patuloy na edukasyon upang makasabay sa mga update at mga bagong feature. Ang mga regular na refresher courses ay makakatulong na mapanatili ang kahusayan.
3. Suporta sa Gumagamit: Ang pag-aalok ng maaasahang suporta ng user at mga mapagkukunan sa pag-troubleshoot ay mahalaga. Ang isang dedikadong IT support team ay maaaring tumulong sa mga teknikal na isyu at makasagot kaagad ng mga tanong.
4. User-Friendly Design': User-Friendly Design: Ang mga interface ng user-friendly EHR at EMR ay maaaring mabawasan ang curve ng pag-aaral para sa mga propesyonal sa pangangalagang pangkalusugan. Ang mga system na intuitive at mahusay na disenyo ay mas madaling i-navigate at nangangailangan ng mas kaunting pagsasanay.
Ang pagtugon sa mga hamong ito ay napakahalaga para sa pag-maximize ng mga benepisyo ng EHRs at EMRs habang tinitiyak ang privacy at seguridad ng data ng pasyente, nagpo-promote ng interoperability, at pagbibigay-kapangyarihan sa mga propesyonal sa pangangalagang pangkalusugan na sulitin ang mga digital na tool na ito.. Ang pagtagumpayan sa mga hamong ito ay patuloy na magiging pokus para sa mga organisasyon ng pangangalagang pangkalusugan at mga regulatory body habang ang paggamit ng mga elektronikong rekord ng kalusugan ay nagiging lalong mahalaga sa modernong paghahatid ng pangangalagang pangkalusugan.
Ang Electronic Health Records (EHRs) at Electronic Medical Records (EMRs) ay lumitaw bilang backbone ng digital health records, na muling hinuhubog ang healthcare landscape. Binago nila ang pangangalaga ng pasyente, naka -streamline na mga daloy ng trabaho, pinahusay na komunikasyon sa mga nagbibigay ng pangangalagang pangkalusugan, at pinadali na pananaliksik sa groundbreaking. Habang ang mga hamon tulad ng seguridad ng data at interoperability ay nagpapatuloy, ang patuloy na pagsisikap upang matugunan ang mga isyung ito ay patuloy na palakasin ang papel ng mga EHR at EMR sa modernong pangangalaga sa kalusugan. Ang pagtanggap sa mga digital na tool na ito ay hindi lamang isang pagpipilian kundi isang pangangailangan para sa paghahatid ng mahusay, mataas na kalidad na pangangalagang pangkalusugan sa digital age. Ang kanilang pag-aampon ay isang testamento sa pangako ng industriya ng pangangalagang pangkalusugan sa pagbibigay ng pangangalaga sa pasyente-sentrik at pagmamaneho ng pagbabago sa pangangalaga ng kalusugan.
Mga Paggamot sa Kaayusan
Bigyan ang iyong sarili ng oras upang makapagpahinga
Garantisadong Pinakamababang Presyo!

Garantisadong Pinakamababang Presyo!
