
Uterine Fibroids: Causes, Symptoms, Treatment, and more
15 Sep, 2023
 Healthtrip Team
Healthtrip TeamUterine fibroids, though noncancerous, present a significant challenge in women's health. These benign growths in the uterus can impact a woman's reproductive health and overall well-being. Understanding uterine fibroids, their types, treatments, and risks is crucial for women of all backgrounds.
Join us on a journey through the world of uterine fibroids. We'll explore treatment options, from watchful waiting to surgery, and even emerging therapies. This blog empowers women with knowledge, offering insights into this complex condition. Whether you're affected or supporting a loved one, we're here to guide you through uterine fibroids, providing valuable information to help you manage this aspect of women's health.
Transform Your Beauty, Boost Your Confidence
Find the right cosmetic procedure for your needs.

We specialize in a wide range of cosmetic procedures

What Are Uterine Fibroids?
Uterine fibroids are essentially abnormal growths that develop within the muscular wall of the uterus. They are typically round or semi-round in shape and can grow either on the inside of the uterus, on the outer surface, or within the uterine wall itself. These growths are not cancerous, and they can range in size from tiny seedlings to large masses that expand the uterus significantly.
Uterine fibroids are a common gynecological condition, with statistics showing that a substantial number of women will develop them at some point during their reproductive years. While the exact cause of uterine fibroids remains unclear, certain risk factors have been identified, including age (more common in women aged 30-40), family history, and race (more prevalent in African American women). It's essential to note that although anyone with a uterus can develop fibroids, they tend to occur more frequently in specific demographic groups.
Uterine fibroids can affect women of various age groups, but they are most commonly diagnosed in women who are in their 30s and 40s. However, they can develop at any age, including during the teenage years or later in life. The symptoms and treatment options may vary depending on a woman's age, reproductive status, and the size and location of the fibroids.
Causes of Uterine Fibroids
- Genetic Factors: A family history of uterine fibroids can increase one's risk of developing them, suggesting a genetic component in their development.
- Hormonal Influences: Hormones, particularly estrogen and progesterone, are believed to promote fibroid growth. These growths often enlarge during periods of high hormone levels, such as pregnancy, and may shrink after menopause when hormone levels decline.
- Other Factors: While genetics and hormones are key factors, other elements such as obesity and lifestyle may also contribute to the development of uterine fibroids. However, their specific roles are still being researched.
Symptoms of Uterine Fibroids
- Heavy Menstrual Bleeding:
- Menstrual periods characterized by excessive bleeding, often requiring frequent pad or tampon changes.
- Pelvic Pain:
- Dull, aching pelvic pain or pressure, typically in the lower abdomen or pelvis.
- Pain During Intercourse:
- Discomfort or pain experienced during sexual intercourse.
- Frequent Urination:
- Increased urge to urinate, often caused by fibroids pressing on the bladder.
- Infertility or Recurrent Miscarriages:
- Submucosal fibroids can interfere with fertility or cause recurrent pregnancy loss.
- Menstrual Clots:
- Passing large blood clots during menstruation.
- Enlarged Abdomen:
- Some individuals may develop an enlarged abdomen, resembling pregnancy, due to the presence of large fibroids.
Types of Uterine Fibroids
A. Subserosal Fibroids
Subserosal fibroids are fibroids that develop on the outer surface of the uterus, just beneath the serosa (the uterine covering). They tend to grow outward and can sometimes form a stalk-like structure, known as a peduncle. Subserosal fibroids often do not cause significant bleeding but can lead to pelvic pain, pressure, and other discomfort due to their size and location.
B. Intramural Fibroids
Intramural fibroids are the most common type and develop within the muscular wall of the uterus itself. These fibroids can vary in size and number and have the potential to cause symptoms such as heavy menstrual bleeding, pelvic pain, and pressure. Depending on their size and location, intramural fibroids may distort the shape of the uterus.
C. Submucosal Fibroids
Submucosal fibroids are situated just beneath the inner lining (mucosa) of the uterus. They have a tendency to protrude into the uterine cavity, potentially causing heavy menstrual bleeding and fertility issues. Submucosal fibroids are more likely to lead to symptoms such as heavy periods and may require removal, especially if they affect fertility.
Most popular procedures in
Total Hip Replacemen
Upto 80% off
90% Rated
Satisfactory
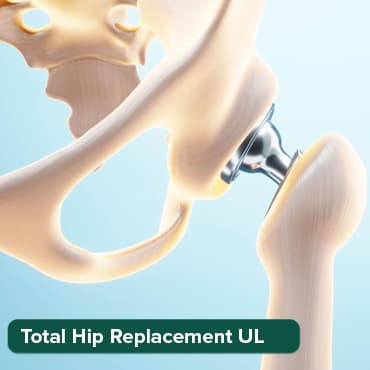
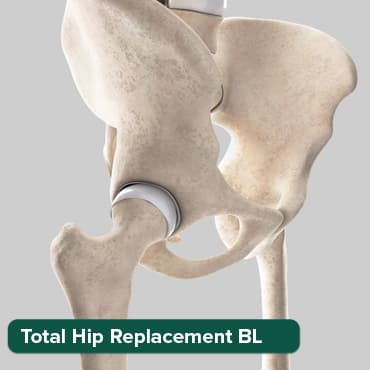
Total Hip Replacemen
Upto 80% off
90% Rated
Satisfactory
Breast Cancer Surger
Upto 80% off
90% Rated
Satisfactory

Total Knee Replaceme
Upto 80% off
90% Rated
Satisfactory
Total Knee Replaceme
Upto 80% off
90% Rated
Satisfactory

D. Pedunculated Fibroids
Pedunculated fibroids are a subtype of subserosal fibroids that grow on a stalk or peduncle, extending away from the uterine wall. These fibroids can sometimes become twisted on their stalk, causing severe pain. Depending on their size and location, pedunculated fibroids may require surgical intervention.
E. Location-Based Classification
Uterine fibroids can also be classified based on their location within the uterus, which includes subserosal, intramural, and submucosal fibroids, as discussed above. This classification helps healthcare providers determine the impact of the fibroids on a woman's health and the most appropriate treatment options.
How are uterine fibroids typically diagnosed
1. Ultrasound:
- Transvaginal Ultrasound: In this procedure, a probe is inserted into the vagina to get a close-up view of the uterus. It's particularly useful for detecting smaller fibroids and their precise location within the uterine wall.
- Abdominal Ultrasound: This involves moving a transducer across the abdominal area to create an image of the uterus and fibroids. It's commonly used and can provide a good overview of fibroid size and location.
2. . MRI (Magnetic Resonance Imaging):
- MRI is a powerful imaging technique that uses magnetic fields and radio waves to create detailed, high-resolution images of the uterus and fibroids.
- It's especially helpful for characterizing the fibroids, determining their exact location, and assessing their impact on surrounding tissues. MRI can aid in treatment planning by providing a comprehensive view of the condition.
3. . Sonohysterography or Hysterosonography:
- Sonohysterography: During this procedure, sterile saline is injected into the uterus to expand the uterine cavity. This expansion allows for a clearer view of the uterine lining and can help identify submucosal fibroids that may be hidden within the uterine wall.
- This technique is often used when traditional ultrasound alone doesn't provide enough detail.
4. Hysteroscopy:
- Hysteroscopy is a minimally invasive procedure where a hysteroscope, a thin, lighted tube with a camera, is gently inserted through the cervix and into the uterus.
- This allows the healthcare provider to directly visualize the inside of the uterus and identify any fibroids within the uterine cavity. It's particularly useful for diagnosing submucosal fibroids and may be combined with therapeutic procedures like fibroid removal if necessary.
These diagnostic methods collectively offer a comprehensive evaluation of uterine fibroids, including their size, location, and impact on the uterine cavity. Accurate diagnosis is crucial for determining the most suitable treatment plan tailored to an individual's unique circumstances. If you suspect you have uterine fibroids or are experiencing symptoms, it's essential to consult a healthcare professional for a proper evaluation and diagnosis.
Treatment Options for Uterine Fibroids
A. Watchful Waiting and Lifestyle Changes
- Watchful Waiting: For women with small fibroids that aren't causing significant symptoms, a "watch and wait" approach may be recommended. Regular monitoring through check-ups and imaging studies can help track fibroid growth and assess if intervention is necessary.
- Lifestyle Changes: Adopting a healthy lifestyle, including maintaining a balanced diet, regular exercise, and stress management, can help manage symptoms and improve overall well-being for some individuals.
B. Medications for Symptom Management
- Pain Relievers: Over-the-counter or prescription pain medications can help alleviate menstrual cramps and pelvic pain associated with fibroids.
- Hormonal Therapies: Hormonal medications, such as birth control pills, intrauterine devices (IUDs) with hormones, or hormonal injections, can regulate heavy menstrual bleeding and reduce pain associated with fibroids.
C. Minimally Invasive Procedures
- Uterine Artery Embolization (UAE): UAE involves blocking the blood supply to fibroids, causing them to shrink. It is a less invasive alternative to surgery and can help alleviate symptoms.
- Myomectomy: Myomectomy is a surgical procedure to remove fibroids while preserving the uterus. It is often recommended for women who wish to retain their fertility.
D. Surgical Options
- Hysterectomy: In cases of severe symptoms or when other treatments are ineffective, a hysterectomy may be recommended. This involves the complete removal of the uterus and is considered a permanent solution for fibroids. In some cases, the ovaries and fallopian tubes may also be removed.
E. Emerging Treatments and Their Efficacy
- MRI-Guided Focused Ultrasound Surgery (MRgFUS): This noninvasive procedure uses high-intensity ultrasound waves to heat and destroy fibroid tissue. It can be an option for some women with symptomatic fibroids.
- Gonadotropin-Releasing Hormone (GnRH) Agonists: These drugs temporarily shrink fibroids by suppressing hormone production but are typically used for short-term relief or before surgery to make removal easier.
- Endometrial Ablation: This procedure destroys the lining of the uterus and may help manage heavy menstrual bleeding caused by small fibroids.
It's essential to discuss treatment options with a healthcare provider to determine the most suitable approach based on the individual's symptoms, the size and location of the fibroids, and the patient's reproductive goals.
Risks and Complications
- Menstrual problems:
- Heavy menstrual bleeding (menorrhagia)
- Prolonged periods
- Irregular menstruation
- Pelvic pain and discomfort:
- Chronic pelvic pain
- Feeling of fullness in the lower abdomen
- Pressure in the pelvic region
- Pain during sexual intercourse:
- Discomfort or pain during sex
- Impact on sexual health and relationships
- Pregnancy complications:
- Fertility issues
- Miscarriage risk
- Preterm birth risk
- Increased likelihood of needing a C-section
- Urinary problems:
- Frequent urination
- Difficulty emptying the bladder
- Increased risk of urinary tract infections (UTIs)
- Gynecological complications:
- Potential association with conditions like pelvic inflammatory disease (PID), endometriosis, or adenomyosis
- Red degeneration (rare but serious):
- Severe abdominal pain
- Fever
- Requires immediate medical attention
It's important to note that not all individuals with uterine fibroids will experience these complications, and the severity of symptoms and risks can vary widely. Seeking medical attention and discussing your specific situation with a healthcare provider is essential for proper management and treatment.
What is the Cost of Treating Uterine Fibroids?
The cost of treating uterine fibroids in India can range from Rs. 50,000 to several lakh rupees or more, depending on the type of treatment, severity of the fibroids, and location of the healthcare provider.
Non-surgical treatments, such as medication and uterine artery embolization (UAE), are generally less expensive than surgical treatments, such as myomectomy and hysterectomy.
In brief, uterine fibroids, though common, can bring about complications such as heavy bleeding, pelvic pain, and fertility concerns. Early diagnosis and tailored treatment are key to mitigating these issues and improving overall well-being. If you suspect uterine fibroids might be affecting you, seek medical advice for personalized care.
Wellness Treatment
Give yourself the time to relax
Lowest Prices Guaranteed!

Lowest Prices Guaranteed!





