
Knowing the Landscape of Spondylolisthesis Surgery
19 Oct, 2023
 Healthtrip Team
Healthtrip TeamSpondylolisthesis Surgery
Spondylolisthesis is a condition where one vertebra slips forward over another, often causing back pain and discomfort. Picture your spine as a stack of building blocks. When one block shifts out of place, it's like spondylolisthesis – a condition that affects the alignment of the spine.Surgery is considered when other treatments fall short, and the slip in the spine is causing significant pain, hindering daily activities.
Transform Your Beauty, Boost Your Confidence
Find the right cosmetic procedure for your needs.

We specialize in a wide range of cosmetic procedures

Why Spondylolisthesis Surgery is Done ?
A. Failed Conservative Treatments: If methods like physical therapy or medications haven't provided relief, surgery may be the next step to address the issue directly.
B. Severe Pain and Functional Impairment: When the pain becomes too intense and starts affecting your ability to move, work, or enjoy life, surgery may offer a more lasting solution.
C. Neurological Symptoms: If spondylolisthesis is pressing on nerves, causing tingling or weakness in the legs, surgery can relieve this pressure and prevent further damage.
D. Types of Spondylolisthesis that Require Surgery: Certain types of spondylolisthesis, especially those at higher grades, may necessitate surgical intervention for stability and pain management.
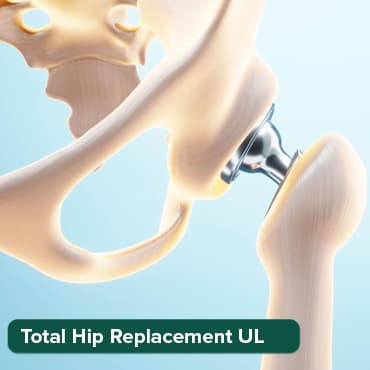
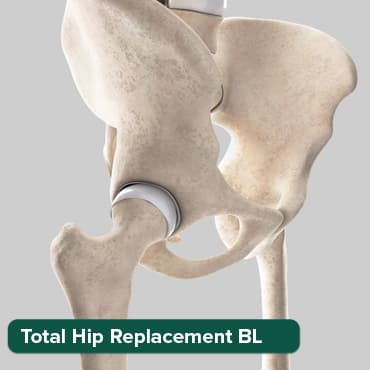
Most popular procedures in India
Total Hip Replacemen
Upto 80% off
90% Rated
Satisfactory
Total Hip Replacemen
Upto 80% off
90% Rated
Satisfactory
Total Hip Replacemen
Upto 80% off
90% Rated
Satisfactory

ANGIOGRAM
Upto 80% off
90% Rated
Satisfactory

ASD Closure
Upto 80% off
90% Rated
Satisfactory

Who Needs Spondylolisthesis Surgery
A. Patient Selection Criteria: Not everyone with spondylolisthesis needs surgery. Those considered for surgery are typically individuals with persistent and severe symptoms despite trying other treatments.
B. Evaluation by Medical Professionals: Your healthcare team will assess your overall health, the extent of the slip, and the impact on your daily life to determine if surgery is the best course of action.
C. Consideration of Age and Health Status: Factors such as age and general health are considered to ensure that surgery is a safe and beneficial option for the individual.
Understanding spondylolisthesis and the reasons for surgery helps individuals make informed decisions about their healthcare journey.
Procedure Overview
A. Preoperative Preparation
1. Diagnostic Tests and Imaging:
Before the surgery, your healthcare team will conduct a series of diagnostic tests and imaging studies to thoroughly assess your condition. This may include X-rays, CT scans, or MRI scans to provide detailed images of the spine. These tests help the surgeon understand the extent of the spondylolisthesis, identify any associated spinal issues, and plan the surgical approach.
2. Consultation with Surgeon and Anesthesiologist:
You'll have in-depth discussions with both your surgeon and anesthesiologist. The surgeon will explain the specific surgical procedure, including potential risks and benefits. This is an opportunity for you to ask questions and address any concerns. The anesthesiologist will review your medical history to ensure that the chosen anesthesia is safe for you. They will also discuss the options for pain management during and after the surgery.
3. Medication Adjustments:
If you are on any medications, your healthcare team may make adjustments based on the upcoming surgery. Certain medications, like blood thinners, may need to be temporarily stopped before the procedure to reduce the risk of excessive bleeding. Your team will provide clear instructions on which medications to continue or discontinue and when to make these adjustments.
4. Physical Condition and Nutrition:
Your overall physical health is crucial for a successful surgery and recovery. Your healthcare team may advise you on exercises to strengthen your body, improving your resilience. Nutrition plays a role too, and you may be guided on maintaining a balanced diet to support healing.
5. Psychological Preparation:
Surgery can be mentally challenging. Preoperative preparation includes addressing any anxiety or stress you may have. Understanding the procedure, knowing what to expect, and having a realistic outlook on the recovery process can significantly contribute to a positive mental state.
6. Advance Care Planning:
It's essential to plan for the postoperative period. Arrange for someone to assist you at home, ensure you have the necessary supplies, and follow any specific preoperative instructions, such as fasting before surgery.
During Surgery
1. Anesthesia Administration:
Before the surgical procedure begins, the anesthesia team will administer anesthesia to ensure that you are comfortable and pain-free throughout the surgery. The type of anesthesia used depends on various factors, including the nature of the surgery, your overall health, and your preferences.
- General Anesthesia: You will be unconscious and completely unaware during the surgery.
- Regional Anesthesia: Numbing specific regions of your body, often used for spinal surgeries.
- Local Anesthesia: Numbing a small, specific area, commonly used in minimally invasive procedures.
The anesthesia team closely monitors your vital signs throughout the surgery to ensure your safety and well-being.
2. Surgical Approaches (e.g., Decompression, Fusion):
- Decompression: If spinal nerves are compressed, a decompression procedure may be performed. This involves removing portions of bone or tissue to relieve pressure on the nerves. Techniques such as laminectomy or foraminotomy may be used, depending on the specific conditions of your spine.
- Fusion:
Fusion is a procedure to stabilize the spine by joining two or more vertebrae together. It is often done using bone grafts and may involve the use of metal implants. Different techniques for fusion include:
- Posterior Fusion: Accessed through the back.
- Anterior Fusion: Accessed through the front.
- Lateral Fusion: Accessed from the side.
The choice of approach depends on the location and severity of the spondylolisthesis, as well as the surgeon's preference and the patient's anatomy.
3. Use of Surgical Instruments and Implants:
- Surgical Instruments: During the procedure, the surgeon uses specialized instruments to perform precise actions. These instruments may include microscopes, drills, and precision tools to ensure accuracy in bone removal, decompression, and fusion processes.
- Implants: Implants are often used to stabilize the spine during fusion. Commonly used implants include screws, rods, and interbody cages. These implants provide support and help maintain proper alignment of the spine during the healing process.
- Bone Grafts: To promote fusion, bone grafts may be used. These grafts can be taken from the patient's own body (autograft) or obtained from a donor (allograft). Bone grafts stimulate the growth of new bone, facilitating the fusion of the vertebrae.
After Spondylolisthesis Surgery
A. Immediate Postoperative Care
1. Wound Care: After surgery, the incision site requires careful attention to prevent infection and promote healing.
- Dressing Changes: The surgical team will instruct you on how to change dressings and keep the incision clean.
- Signs of Infection: Watch for signs of infection, such as increased redness, swelling, or drainage from the wound.
2. Physical Therapy Initiation: Early mobilization and physical therapy are crucial for recovery.
- Assisted Ambulation: Depending on the surgery, you may start with assisted walking and gradually progress to independent mobility.
- Range of Motion Exercises: Physical therapy will include exercises to improve flexibility and prevent stiffness.
- Pain Management: Therapists will guide you on managing pain during movement.
3. Monitoring for Complications: Immediate postoperative monitoring helps detect and address complications promptly.
- Neurological Monitoring: Assessing nerve function to ensure there's no new weakness or numbness.
- Pain Management: Regular assessment of pain levels to adjust medications accordingly.
- Vital Signs Monitoring: Continuous monitoring of vital signs such as heart rate, blood pressure, and oxygen levels.
B. Rehabilitation and Recovery
1. Physical Therapy Programs: Tailored physical therapy is essential for regaining strength and function.
- Core Strengthening: Focus on strengthening the core muscles to support the spine.
- Gait Training: Assistance in developing a proper walking pattern to avoid strain on the spine.
- Functional Activities: Exercises simulating daily activities to enhance overall functionality.
2. Activity Restrictions: While recovery progresses, certain activities may be restricted to protect the healing spine.
- Lifting Restrictions: Avoid heavy lifting to prevent strain on the spine.
- Bending and Twisting: Minimize movements that strain the back during the initial recovery period.
- Gradual Resumption: Activities will be gradually reintroduced based on healing progress.
3. Follow-up Appointments: Regular follow-up appointments are crucial for monitoring recovery and addressing any concerns.
- Imaging Studies: Periodic X-rays or other imaging studies may be conducted to assess fusion progress.
- Medication Adjustments: Pain medications may be adjusted based on your pain levels.
Latest Advancements in Spondylolisthesis Surgery
A. Minimally Invasive Techniques:
Recent advancements have focused on minimizing the impact of surgery on the body.
- Small Incisions: Minimally invasive procedures involve smaller incisions, reducing tissue damage.
- Endoscopic Approaches: Use of endoscopes for visualization, allowing surgeons to perform procedures with enhanced precision.
- Faster Recovery: Patients often experience shorter hospital stays and faster recovery times.
B. Robotic-Assisted Surgeries:
Robotics has entered the field of spinal surgery, enhancing precision and control.
- Enhanced Precision: Robots assist surgeons in performing precise movements during surgery.
- Image-Guided Navigation: 3D imaging and navigation systems help guide the robotic tools accurately.
- Customization: Surgeons can tailor procedures to the patient's anatomy with greater accuracy.
C. Advancements in Implant Technology:
Implant technology continues to evolve, contributing to better outcomes and increased stability.
- Biocompatible Materials: Implants made from materials that promote bone growth and fusion.
- Dynamic Implants: Adaptive implants that allow for controlled movement, mimicking the natural spine.
- Improved Durability: Long-lasting materials that reduce the need for revision surgeries.
Tips for Preparing Yourself for Spondylolisthesis Surgery
- Learn about the procedure, potential outcomes, and recovery to manage expectations.
- Seek emotional support from friends, family, or support groups.
- Consider counseling or mindfulness practices to manage stress.
- Engage in exercises recommended by your healthcare team to strengthen your body.
- Maintain a balanced diet to support overall health and recovery.
- Ensure you are well-rested before the surgery.
- Surround yourself with family and friends who can provide assistance and encouragement.
- Connect with individuals who have undergone similar surgeries to share experiences and tips.
Risks and Complications
A. General Surgical Risks:
- Anesthesia Risks: Complications related to the administration of anesthesia.
- Bleeding: Excessive bleeding during or after surgery.
- Infection: Risk of infection at the surgical site.
B. Specific Risks Associated with Spondylolisthesis Surgery:
- Nerve Damage: Potential damage to nerves during the procedure.
- Failed Fusion: Fusion may not occur as expected, requiring additional interventions.
- Instrument Failure: Rare instances of implant or hardware failure.
C. Infection Prevention Strategies:
- Sterile Techniques: Surgeons employ strict sterile techniques during surgery.
- Prophylactic Antibiotics: Administration of antibiotics before surgery to prevent infections.
- Postoperative Monitoring: Vigilant monitoring for signs of infection during the recovery period.
In summary, spondylolisthesis surgery combines advanced medical techniques with patient-focused strategies. The preoperative phase involves thorough diagnostics and collaboration, while surgical advancements like minimally invasive approaches and robotics enhance precision. Postoperatively, meticulous care, early therapy, and vigilant monitoring contribute to successful recoveries. Follow-up appointments, clear communication, and patient engagement are paramount. Emotional readiness, physical conditioning, and robust support systems are vital elements, and patient resources and support groups offer valuable communal support. As advancements persist, the integration of cutting-edge techniques with patient-centered care remains pivotal for optimal outcomes and sustained well-being.
Wellness Treatment
Give yourself the time to relax
Lowest Prices Guaranteed!

Lowest Prices Guaranteed!







