
Oncology : The Latest Advances in Cancer Treatments
18 Oct, 2023
 Healthtrip Team
Healthtrip TeamTraditional Cancer Treatments
Transform Your Beauty, Boost Your Confidence
Find the right cosmetic procedure for your needs.

We specialize in a wide range of cosmetic procedures

Traditional cancer treatments have long been the cornerstone in the fight against malignancies, with various modalities aiming to eradicate or control the growth of cancerous cells.
A. Surgery:
1. Tumor Removal Techniques:
Surgical intervention remains a primary method for treating cancer, involving the removal of tumors through various techniques such as excision, resection, and sometimes organ transplantation. Surgeons employ cutting-edge technology and minimally invasive procedures to ensure precision and reduce recovery times.
2. Limitations and Challenges:
Most popular procedures in India
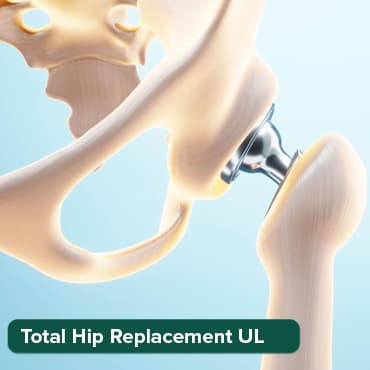
Total Hip Replacemen
Upto 80% off
90% Rated
Satisfactory
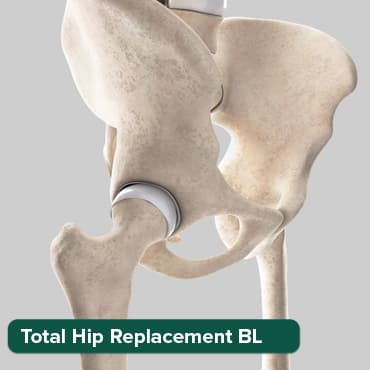
Total Hip Replacemen
Upto 80% off
90% Rated
Satisfactory
Total Hip Replacemen
Upto 80% off
90% Rated
Satisfactory

ANGIOGRAM
Upto 80% off
90% Rated
Satisfactory

ASD Closure
Upto 80% off
90% Rated
Satisfactory

While surgery can be highly effective, its applicability depends on factors like tumor size, location, and the overall health of the patient. Challenges arise when dealing with tumors in critical or hard-to-reach areas, and the invasiveness of the procedure can pose risks and extended recovery periods.
B. Radiation Therapy:
1. External Beam Radiation:
This technique involves directing high-energy rays from an external source towards the cancerous site, precisely targeting the tumor while minimizing damage to surrounding healthy tissue. It is a crucial component in treating localized cancers and is often employed post-surgery to eliminate remaining cancer cells.
2. Internal Radiation (Brachytherapy):
Brachytherapy involves placing a radiation source directly inside or very close to the tumor, delivering a concentrated dose of radiation. This method is particularly useful in treating prostate, cervical, and breast cancers. Advances in imaging technology have enhanced the precision of brachytherapy.
3. Side Effects and Improvements:
Radiation therapy may cause side effects such as fatigue, skin changes, or nausea. Technological advancements, including intensity-modulated radiation therapy (IMRT) and proton therapy, aim to minimize collateral damage to healthy tissues, thus reducing side effects and improving overall treatment outcomes.
C. Chemotherapy:
1. Systemic Chemotherapy:
This approach involves the use of drugs that circulate throughout the body, targeting rapidly dividing cancer cells. While effective, systemic chemotherapy often affects healthy cells, leading to side effects such as hair loss and immunosuppression.
2. Targeted Therapy:
Targeted therapies focus on specific molecules involved in cancer growth, minimizing harm to normal cells. These therapies, like tyrosine kinase inhibitors and monoclonal antibodies, mark a paradigm shift towards more precise and less toxic treatments.
3. Evolution of Chemotherapy Regimens:
The field of chemotherapy continues to evolve, with researchers exploring novel drug combinations and treatment schedules. Personalized medicine, guided by genetic profiling, allows for tailored chemotherapy regimens based on individual patient characteristics, optimizing effectiveness and minimizing side effects.
In the ever-evolving landscape of cancer treatment, these traditional methods persist as crucial pillars, continually refined and complemented by innovative approaches for a more effective and patient-friendly therapeutic arsenal.
Advances in cancer treatments
1. Precision Medicine:
Precision medicine has helped to improve outcomes for patients with many types of cancer, including lung cancer, colon cancer, and leukemia. [Source: National Cancer Institute]
A. Genomic Profiling in Cancer Treatment:
1. Next-Generation Sequencing (NGS):
Next-generation sequencing technologies have revolutionized our ability to analyze the genomic landscape of cancer. NGS enables the rapid and cost-effective sequencing of large portions of the genome, facilitating the identification of genetic mutations and alterations associated with cancer development.
2. Identifying Genetic Mutations and Alterations:
Genomic profiling allows for a comprehensive analysis of a patient's tumor DNA. This includes identifying mutations in key cancer-related genes, understanding the genomic heterogeneity of tumors, and uncovering potential targets for personalized therapies.
B. Personalized Treatment Approaches:
Tailoring Therapies Based on Genetic Profiles: Precision medicine involves customizing treatment strategies based on the unique genetic makeup of an individual's cancer. By understanding the specific mutations driving the cancer, clinicians can choose therapies that target those particular abnormalities, leading to more effective and less toxic treatments.
Benefits:
- Enhanced Treatment Efficacy: Tailoring treatments to the genetic profile of the tumor can lead to higher response rates and better outcomes.
- Reduced Side Effects: Precision medicine aims to minimize harm to healthy tissues, potentially reducing the side effects associated with traditional, one-size-fits-all treatments.
- Optimized Drug Selection: Genomic profiling assists in identifying drugs that are more likely to be effective, avoiding unnecessary exposure to ineffective therapies.
Limitations:
- Genomic Complexity: Tumors are genetically complex, and identifying all relevant mutations can be challenging. Moreover, the significance of some mutations may not be well understood.
- Resistance and Adaptation: Tumors can evolve over time, developing resistance to initially effective therapies. Continuous monitoring and adaptation of treatment plans are essential.
- Cost and Accessibility: While the cost of genomic profiling has decreased, it remains a factor, and accessibility to these advanced technologies can be a challenge for some patients and healthcare systems.
Precision medicine, guided by genomic profiling, heralds a new era in cancer treatment by moving beyond one-size-fits-all approaches. The ability to tailor therapies based on individual genetic profiles brings both promise and complexity, necessitating ongoing research and clinical collaboration to unlock its full potential in improving patient outcomes
Immunotherapy:
A. Immunotherapy:
- Key Principles: Immunotherapy harnesses the body's immune system to combat cancer. Unlike traditional treatments, it focuses on enhancing the natural defenses of the body.
- Activation of the Immune System Against Cancer Cells: Immunotherapy stimulates the immune response by recognizing and attacking cancer cells. This can involve boosting T-cell activity, promoting the production of cytokines, or enhancing the ability of immune cells to identify and eliminate cancerous cells.
B. Immune Checkpoint Inhibitors:
1. PD-1/PD-L1 Inhibitors: Programmed cell death protein 1 (PD-1) and its ligand PD-L1 are checkpoints that cancer cells exploit to evade the immune system. Inhibitors like pembrolizumab and nivolumab block these checkpoints, allowing T cells to recognize and attack cancer cells effectively.
2. CTLA-4 Inhibitors: Cytotoxic T-lymphocyte-associated protein 4 (CTLA-4) is another checkpoint that hampers immune response. Inhibitors like ipilimumab unleash the immune system by blocking CTLA-4, enabling a more robust anti-cancer response.
C. CAR-T Cell Therapy:
1. Engineering T Cells for Cancer Targeting:
Chimeric Antigen Receptor T-cell (CAR-T) therapy involves genetically modifying a patient's T cells to express a receptor that recognizes specific cancer antigens. This modification enables T cells to target and destroy cancer cells more effectively.
2. Successes and Challenges:
CAR-T therapy has shown remarkable success, particularly in treating certain blood cancers. However, challenges include managing side effects such as cytokine release syndrome and addressing issues related to the persistence and durability of the engineered T cells.
D. Monoclonal Antibodies:
1. Mechanism of Action:
Monoclonal antibodies are laboratory-created molecules that mimic the immune system's ability to fight off harmful pathogens. They can target specific proteins on the surface of cancer cells, tagging them for destruction by the immune system or interfering with their ability to grow and divide.
2. Recent Developments and Applications:
Advances in monoclonal antibody therapy include the development of bispecific antibodies, capable of targeting multiple cancer antigens simultaneously. Monoclonal antibodies find applications in various cancers, ranging from breast cancer to leukemia, showcasing their versatility and expanding therapeutic possibilities.
Immunotherapy represents a paradigm shift in cancer treatment, leveraging the body's own defenses to combat the disease. From immune checkpoint inhibitors that release the brakes on immune cells to CAR-T cell therapy that engineers T cells for precise cancer targeting, these approaches signify a new era in oncology with unprecedented successes and ongoing research to address challenges and broaden the scope of immunotherapeutic applications.
Nanotechnology in Cancer Treatment:
A. Introduction to Nanotechnology:
1. Nanoparticles and Their Applications:
Nanotechnology involves manipulating materials at the nanoscale (typically between 1 and 100 nanometers) to exploit unique properties. In cancer treatment, nanoparticles, often made of materials like lipids or polymers, are designed for specific applications such as drug delivery, imaging, and diagnostics. Their small size and large surface area-to-volume ratio offer advantages in interacting with biological systems.
2. Drug Delivery Systems:
Nanoparticles serve as advanced drug delivery vehicles, carrying therapeutic agents directly to cancer cells. This targeted delivery minimizes damage to healthy tissues, enhances drug bioavailability, and allows for controlled release, optimizing the therapeutic effect while reducing side effects associated with traditional chemotherapy.
B. Theranostics:
1. Simultaneous Diagnosis and Treatment using Nanotechnology:
Theranostics is a rapidly advancing field that combines therapeutic and diagnostic capabilities within a single platform. Nanoparticles in theranostics enable simultaneous imaging of cancer cells and the delivery of therapeutic agents. This dual functionality allows for real-time monitoring of treatment response and adjustments, fostering a more personalized and precise approach to cancer therapy.
2. Future Prospects:
The future of nanotechnology in cancer theranostics holds immense promise. Anticipated developments include:
- Multifunctional Nanoparticles: Continued exploration of nanoparticles with multiple functions, such as imaging, drug delivery, and targeted therapy, to create comprehensive and adaptable treatment platforms.
- Smart Nanosystems: Development of smart nanosystems capable of responding to specific cues within the tumor microenvironment, enhancing targeted drug release and treatment efficacy.
- Biosensors and Imaging Agents: Integration of advanced biosensors and imaging agents into nanoparticles for early detection, monitoring treatment response, and predicting disease progression.
- Combination Therapies: Exploration of combinations of different nanoparticles or hybrid systems for synergistic therapeutic effects, addressing the heterogeneity of cancer cells and minimizing the risk of resistance.
- Clinical Translation: Increasing efforts to translate promising nanotechnological approaches from the laboratory to clinical settings, bringing these innovative therapies closer to mainstream cancer care.
Nanotechnology's integration into cancer treatment showcases a remarkable convergence of science and medicine. The versatility of nanoparticles in drug delivery and the simultaneous diagnostic capabilities of theranostic platforms open new frontiers in the pursuit of effective, targeted, and personalized cancer therapies. As researchers delve deeper into these nanoscale realms, the future holds exciting possibilities for transforming the landscape of cancer treatment.
Hyperthermia and Radiofrequency Ablation:
A. Localized Heating for Cancer Treatment:
Localized heating, or hyperthermia, is a therapeutic approach that involves raising the temperature of specific tissues or regions within the body to enhance the effectiveness of cancer treatment.
1. Principles of Localized Heating: Hyperthermia exploits the sensitivity of cancer cells to elevated temperatures, which can induce cell death or sensitize them to radiation and chemotherapy. This approach aims to selectively target cancer cells while minimizing damage to surrounding healthy tissues.
2. Methods of Inducing Hyperthermia: Techniques for inducing hyperthermia include external methods like focused ultrasound or microwave applicators, as well as internal methods such as probes inserted directly into tumors. The choice of method depends on the location and size of the tumor.
B. Radiofrequency Ablation Techniques:
Radiofrequency ablation (RFA) is a specific form of hyperthermia that employs high-frequency electrical currents to generate heat and destroy cancer cells.
1. Procedure:
During RFA, a specialized needle or electrode is inserted into the tumor, guided by imaging techniques such as ultrasound or CT scans. Radiofrequency energy is then applied, heating the tissue and causing coagulative necrosis, effectively destroying the cancerous cells.
2. Applicability:
RFA is commonly used for treating solid tumors, particularly in the liver, lung, kidney, and bone. It is a minimally invasive procedure that can be performed percutaneously or during surgery.
C. Advantages and Challenges:
1. Advantages:
- Minimally Invasive: RFA is often a minimally invasive procedure, reducing the need for extensive surgery and allowing for quicker recovery times.
- Local and Focused Treatment: Hyperthermia and RFA enable localized treatment, minimizing damage to surrounding healthy tissues.
- Repeatable: In some cases, RFA can be repeated if necessary, offering a potential option for recurrent tumors.
- Combination with Other Therapies: RFA can be used in conjunction with other treatments, such as surgery or chemotherapy, to enhance overall therapeutic effectiveness.
2. Challenges:
- Tumor Size and Location: The effectiveness of RFA may be limited by the size and location of the tumor. Larger tumors or those near critical structures may be challenging to treat.
- Incomplete Ablation: Ensuring complete ablation of the tumor while avoiding damage to adjacent tissues can be complex and may require careful planning and monitoring.
- Heat Dissipation: The efficiency of RFA can be affected by factors such as blood flow, which can dissipate heat and limit the treatment's effectiveness.
- Patient Selection: Not all patients or tumor types are suitable for hyperthermia or RFA, and careful patient selection is crucial for optimal outcomes.
Hyperthermia and radiofrequency ablation represent innovative approaches in the arsenal of cancer treatment modalities. Their localized and focused nature, coupled with the potential for minimal invasiveness, underscores their significance in providing alternative options for patients, particularly in cases where traditional treatments may be less feasible or effective. However, ongoing research is essential to refine techniques and expand the applicability of these therapies in diverse cancer scenarios.
Advances in Early Detection:
A. Liquid Biopsy:
1. Detection of Circulating Tumor DNA (ctDNA):
- Principle: Liquid biopsy involves the analysis of genetic material, such as ctDNA, circulating in bodily fluids like blood. ctDNA carries genetic information from tumor cells, allowing for the identification of specific mutations associated with cancer.
- Early Detection: Liquid biopsy offers a non-invasive method for detecting cancer at an early stage by identifying genetic alterations indicative of tumor presence. This is particularly valuable for cancers where traditional screening methods may be limited.
- Disease Monitoring: It provides a dynamic picture of the tumor's genetic landscape, enabling real-time monitoring of changes in genetic profiles and treatment responses.
2. Non-Invasive Monitoring of Treatment Response:
- Dynamic Assessment: Liquid biopsy allows for the continuous monitoring of treatment response by tracking changes in ctDNA over time. This dynamic assessment can help clinicians tailor treatment strategies based on the evolving genetic profile of the tumor.
- Minimizing Invasive Procedures: Compared to traditional tissue biopsies, liquid biopsies reduce the need for invasive procedures, providing a less burdensome and more patient-friendly approach to monitoring disease progression and treatment efficacy.
B. Artificial Intelligence in Imaging:
1. Improving Diagnostic Accuracy:
- Image Analysis: Artificial intelligence (AI) algorithms can analyze medical imaging data, including CT scans, MRIs, and mammograms, with unprecedented speed and accuracy.
- Early Lesion Detection: AI has the potential to detect subtle abnormalities or lesions that may be challenging for human observers, thereby improving the sensitivity of early cancer detection.
- Reducing False Positives and Negatives: By fine-tuning diagnostic accuracy, AI can help reduce both false positives and false negatives, improving overall diagnostic reliability.
2. Applications in Radiology:
- Automated Image Interpretation: AI algorithms can assist radiologists in interpreting images, expediting the diagnostic process and allowing for more efficient patient care.
- Risk Stratification: AI can aid in stratifying patients based on their risk profile, helping healthcare providers prioritize individuals who may benefit most from additional screening or surveillance.
- Integration with Clinical Data: AI systems can integrate imaging data with other clinical information, providing a comprehensive view of a patient's health and aiding in personalized treatment planning.
Advances in early detection, driven by liquid biopsy and AI in imaging, represent a paradigm shift in cancer care .
Emerging Technologies:
- CRISPR-Based Therapies: The revolutionary CRISPR technology offers precise gene editing, holding potential for tailored cancer treatments.
- Advancements in Cancer Vaccines: Ongoing advancements in cancer vaccines aim to leverage the immune system for prevention and treatment, marking a promising frontier in cancer research.
In brief, recent advances in cancer treatment, from immunotherapy to precision medicine and innovative technologies like liquid biopsy and artificial intelligence, offer significant strides toward more effective and personalized care. This collective progress instills optimism for a future where cancer is not only better managed but potentially preventable. However, the journey continues, calling for ongoing research, collaboration, and a shared commitment to translating these advancements into transformative therapies. The evolving landscape promises a future defined by resilience, hope, and the triumph over cancer.
Wellness Treatment
Give yourself the time to relax
Lowest Prices Guaranteed!

Lowest Prices Guaranteed!







