
مرض الشريان التاجي: من الأعراض إلى الإدارة
08 Aug, 2023
 فريق هيلث تريب
فريق هيلث تريبيعد مرض الشريان التاجي (CAD)، الذي غالبًا ما يكون مرادفًا لمرض نقص تروية القلب، أحد أكثر أمراض القلب والأوعية الدموية انتشارًا وتأثيراً في جميع أنحاء العالم.. يتميز مرض الشريان التاجي في جوهره بتراكم لويحات تصلب الشرايين داخل الشرايين التاجية، وهي الأوعية الحيوية المسؤولة عن إمداد عضلة القلب بالدم الغني بالأكسجين. مع تطور هذه اللوحات وتصلبها ، يمكن أن تعيق تدفق الدم ، مما يؤدي إلى مجموعة من المظاهر السريرية التي تتراوح من آلام الصدر (الذبحة الصدرية) إلى أحداث أكثر شدة مثل النوبات القلبية. نشأة CAD متعددة الأوجه ، تتشابك في الاستعدادات الوراثية مع عوامل الخطر القابلة للتعديل مثل النظام الغذائي ، والنشاط البدني ، واستخدام التبغ. بالنظر إلى تأثيرها العميق على الصحة العالمية ، فإن فهم تعقيدات CAD ، من الفيزيولوجيا المرضية إلى إدارتها ، أمر بالغ الأهمية لكل من أخصائيي الرعاية الصحية والجمهور العام.
تحويل جمالك، تعزيز ثقتك بنفسك
العثور على مستحضرات التجميل المناسبة الإجراء لاحتياجاتك.

نحن متخصصون في مجموعة واسعة من إجراءات التجميل

مرض الشريان التاجي (CAD)
يشير مرض الشريان التاجي (CAD)، المعروف أيضًا باسم مرض القلب الإقفاري، إلى حالة تتراكم فيها الترسبات في الشرايين التاجية، التي تزود عضلة القلب بالدم الغني بالأكسجين. يمكن أن يؤدي هذا التراكم إلى تضييق الشرايين وتقليل تدفق الدم إلى القلب، مما يؤدي إلى أمراض قلبية مختلفة مثل الذبحة الصدرية أو النوبات القلبية.
أهمية الشرايين التاجية في وظيفة القلب:
تلعب الشرايين التاجية دورًا محوريًا في ضمان حصول القلب على الأكسجين والمواد المغذية التي يحتاجها ليعمل بفعالية. أي حل وسط في صلاحيتها أو وظيفتها يمكن أن يكون له آثار كبيرة على الصحة العامة وكفاءة القلب.
الإجراءات الأكثر شعبية في الهند
استبدال الورك الكلي
خصم يصل إلى 80%
تقييم 90%
مرض
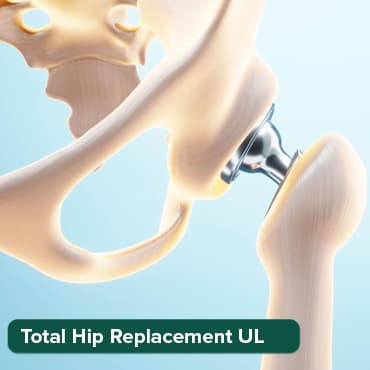
استبدال الورك الكلي
خصم يصل إلى 80%
تقييم 90%
مرض
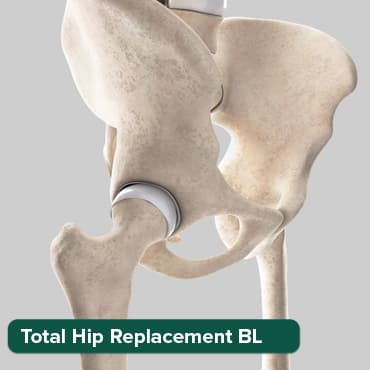
استبدال الورك الكلي-
خصم يصل إلى 80%
تقييم 90%
مرض

أنجيوجرام
خصم يصل إلى 80%
تقييم 90%
مرض

إغلاق ASD
خصم يصل إلى 80%
تقييم 90%
مرض

على الصعيد العالمي، CAD هو السبب الرئيسي للوفاة. وتقدر منظمة الصحة العالمية ذلك 17.9 تحدث مليون حالة وفاة كل عام بسبب أمراض القلب والأوعية الدموية ، والتي تعد CAD مساهماً مهمًا. يختلف انتشار المرض على المستوى الإقليمي، حيث ترتفع المعدلات في الدول الغربية، لكنه أصبح مصدر قلق متزايد في الدول النامية أيضًا.
أعراض CAD
- الذبحة الصدرية (ألم في الصدر): غالبًا ما يوصف بأنه الضغط ، والثقل ، والضيق ، والضغط ، أو الحرق ، أو المؤلم خلف عظمة الثدي. ينتشر هذا الألم غالبًا إلى الرقبة أو الفك أو الذراعين أو الكتفين أو الحلق أو الظهر أو حتى الأسنان.
- ضيق في التنفس: إذا لم يتمكن القلب من ضخ ما يكفي من الدم لتلبية احتياجات الجسم، فقد يظهر ذلك على شكل ضيق في التنفس مع المجهود أو أثناء الراحة.
- تعب: أقل شيوعًا ، لكن بعض الناس يعانون من التعب الشديد أو انخفاض القدرة على أداء الأنشطة الروتينية.
- الخفقان: عدم انتظام ضربات القلب، أو الشعور بتخطي نبضات القلب.
- الضعف أو الدوخة: يمكن أن يؤدي عدم تدفق الدم بشكل كافٍ إلى حدوث نوبات من الضعف أو الدوخة أو الإغماء.
- غثيان: يمكن أن يحدث ، غالبًا مع أو بدون ألم في الصدر.
- التعرق: قد تصاحب الأعراض المذكورة أعلاه ، وغالبًا ما يشار إليها باسم "العرق البارد."
- بدون أعراض ظاهرة: قد لا يعاني بعض الأفراد من أي أعراض على الإطلاق، وهي حالة تعرف باسم CAD "الصامت.
أسباب وعوامل الخطر لCAD
عادةً ما يكون السبب الجذري لمرض الشريان التاجي هو تصلب الشرايين، وهو تراكم الكوليسترول والمواد الأخرى على الجدران الداخلية للشرايين. تتأثر هذه العملية بعدة عوامل خطر:
- مستويات الكولسترول في الدم غير الصحية: وهذا يشمل مستويات عالية من الكوليسترول البروتين الدهني منخفض الكثافة (LDL) (الكوليسترول "السيئ) ومستويات منخفضة من الكوليسترول البروتين الدهني (HDL) عالي الكثافة (HDL) (الكوليسترول" "جيد).
- ضغط دم مرتفع: يزيد من عبء العمل على القلب، مما يتسبب في زيادة سماكة عضلة القلب وتصلبها.
- التدخين: المواد الكيميائية في التبغ يمكن أن تلحق الضرر بالأوعية الدموية.
- مقاومة الأنسولين أو مرض السكري: مع مرض السكري، يرتفع مستوى السكر في الدم، مما قد يؤدي إلى تسريع تصلب الشرايين.
- السمنة أو الوزن الزائد: يمكن أن تزيد الدهون الزائدة، خاصة حول الخصر، من خطر الإصابة بمرض الشريان التاجي.
- متلازمة الأيض: مجموعة من الحالات بما في ذلك ارتفاع ضغط الدم وارتفاع نسبة السكر في الدم وزيادة الدهون في الجسم حول الخصر ومستويات الكوليسترول غير الطبيعية.
- نمط حياة مستقر: يرتبط عدم ممارسة الرياضة بمرض CAD وعوامل الخطر المرتبطة به.
- نظام غذائي غير صحي:: يمكن أن تسهم الوجبات الغذائية عالية في الدهون المشبعة والدهون غير المشبعة والصوديوم والسكر في تطور CAD.
- التهاب مزمن: يمكن أن تزيد الحالات مثل التهاب المفاصل الروماتويدي أو الذئبة.
- عمر: إن الحصول على كبار السن يزيد من خطر الإصابة بالشرايين التالفة والضيق.
- تاريخ العائلة: التاريخ العائلي لأمراض القلب هو أحد عوامل خطر الإصابة بأمراض القلب التاجية.
- ضغوطالصورة: قد يؤدي التوتر غير المريح إلى إتلاف الشرايين وزيادة عوامل الخطر الأخرى للإصابة بمرض الشريان التاجي.
- Sتوقف التنفس أثناء النوم: توقف التنفس أثناء النوم غير المعالجة يمكن أن يزيد من خطر ارتفاع ضغط الدم وعدم انتظام ضربات القلب والسكتة الدماغية وفشل القلب.
إجراءات التشخيص
1. مساعدة مبدئية
- مقابلة المريض: جمع التاريخ الصحي الشامل والأعراض وعوامل الخطر.
- الفحص البدني: فحص العلامات الحيوية، والاستماع إلى أصوات القلب، وإجراء تقييم عام.
2. الاختبارات التشخيصية الأساسية
- تحاليل الدم: التحقق من مستويات الدهون وعلامات إصابة القلب أو الالتهاب.
- مخطط كهربية القلب أثناء الراحة (ECG): يكتشف إيقاع القلب أو نقص التروية أو النوبات القلبية السابقة.
3. اختبارات التصوير غير الغازية
- مخطط صدى القلب: يقيم بنية القلب والوظيفة.
- ممارسة اختبار الإجهاد: يقيم استجابة القلب للإجهاد البدني.
- التصوير النووي: يقيم تدفق الدم ووظيفة القلب تحت الضغط والراحة.
4. إجراءات التصوير والتشخيص المتقدمة
- تصوير الأوعية التاجية المقطعية: التصوير التفصيلي غير الجراحي لتشريح الشريان التاجي.
- التصوير بالرنين المغناطيسي للقلب: صور تفصيلية لبنية القلب ووظيفته وتوصيف الأنسجة دون الإشعاعات المؤينة.
5. اختبار التشخيص الغازية
- تصوير الأوعية التاجية: قياسي الذهب لتحديد التشريح التاجي وتحديد انسداد محدد.
- الموجات فوق الصوتية داخل الأوعية الدموية (IVUS): يوفر صورة مقطعية للشرايين التاجية.
- احتياطي التدفق الجزئي (FFR): يقيس تدرج الضغط عبر تضييق الشريان التاجي لتقييم تأثيره الفسيولوجي.
بناءً على نتائج هذه الاختبارات، يمكن لطبيب القلب تحديد وجود ومدى وشدة مرض الشريان التاجي ووضع خطة علاج مناسبة، والتي قد تشمل تعديلات نمط الحياة، أو الأدوية، أو إجراءات مثل رأب الأوعية الدموية أو تطعيم مجازة الشريان التاجي (CABG)..
يجب أن تسترشد العملية بدءًا من التقييم الأولي وحتى التشخيص المتقدم بأعراض المريض والنتائج السريرية وعوامل الخطر، مع الموازنة بين الحاجة إلى إجراء تحقيق شامل مع الغزو والمخاطر المرتبطة بإجراءات معينة.
العلاج والإدارة
مرض الشريان التاجي (CAD) هو حالة متعددة الأوجه، وتتطلب إدارتها اتباع نهج شامل يدمج تعديلات نمط الحياة، والعلاج الدوائي، وفي بعض الحالات، التدخلات الغازية. الأهداف الأساسية للعلاج هي تخفيف الأعراض، ووقف أو عكس تطور المرض، والحد من خطر حدوث مضاعفات مثل النوبات القلبية..
1. تعديلات نمط الحياة:
- نظام عذائي: اعتماد نظام غذائي صحي القلب أمر بالغ الأهمية. يتضمن ذلك تناول الأطعمة التي تحتوي على نسبة منخفضة من الدهون المشبعة والمتحولة والكولسترول والصوديوم. وينبغي التركيز على الفواكه والخضروات والحبوب الكاملة والبروتينات الخالية من الدهون. يمكن أن يؤدي تقليل تناول الأطعمة المصنعة والمشروبات السكرية إلى تقليل خطر تصلب الشرايين ومضاعفاته.
- يمارس: النشاط البدني المنتظم يقوي عضلة القلب ، ويحسن الدورة الدموية ، ويساعد على الحفاظ على وزن صحي. من المستحسن للمرضى استشارة مقدم الرعاية الصحية الخاص بهم لتحديد نظام التمارين المناسب، خاصة إذا كانوا يعانون من أعراض قلبية نشطة.
- الإقلاع عن التدخين: التدخين هو عامل خطر رئيسي لCAD. لا يؤدي الإقلاع عن التدخين إلى إبطاء تطور مرض الشريان التاجي فحسب، بل يقلل أيضًا من خطر الإصابة بأمراض القلب والأوعية الدموية الأخرى. يمكن أن تساعد الموارد المختلفة، بما في ذلك الاستشارة والعلاجات ببدائل النيكوتين، في الإقلاع عن التدخين.
2. الأدوية:
- مضادات الصفيحات (ه.ز., أسبرين): تمنع هذه الأدوية تكوين جلطات الدم عن طريق تثبيط تراكم الصفائح الدموية. على سبيل المثال، يوصف الأسبرين عادة لتقليل خطر الإصابة بالنوبات القلبية لدى مرضى CAD.
- حاصرات بيتا: تعمل هذه الأدوية على خفض ضغط الدم ومعدل ضربات القلب، وبالتالي تقليل عبء العمل على القلب. يمكنهم أيضًا تخفيف أعراض الذبحة الصدرية.
- الستاتين: هذه هي الأدوية المخفضة للكوليسترول والتي لا تقلل مستويات الكوليسترول الضار (LDL) فحسب، بل تعمل أيضًا على تثبيت اللويحات الموجودة في الشرايين، مما يقلل من خطر التمزق.
- مثبطات إيس: تعمل هذه الأدوية على خفض ضغط الدم ويمكن أن تقلل الضغط على القلب. لديهم أيضا تأثير وقائي ضد تقدم قصور القلب.
- النترات (ه.ز., النتروجليسرين): هذه الأدوية تمدد الشرايين التاجية ، مما يعزز تدفق الدم إلى عضلة القلب. وهي فعالة بشكل خاص في تخفيف أعراض الذبحة الصدرية الحادة.
3. إجراءات الغازية:
- التدخل التاجي عن طريق الجلد (PCI): يتضمن هذا الإجراء، المعروف باسم رأب الأوعية الدموية، توصيل قسطرة بالبالون إلى الشريان المسدود. يتم نفخ البالون لفتح الانسداد، وغالبًا ما يتم وضع دعامة لإبقاء الشريان مفتوحًا.
- تطعيم مجازة الشريان التاجي (CABG): يتضمن هذا الإجراء الجراحي استخدام وريد أو شريان من جزء آخر من الجسم لتجاوز الشريان التاجي المسدود. إنه مفيد بشكل خاص للمرضى الذين يعانون من شرايين متعددة أو أنماط محددة من الانسداد.
تتطلب الإدارة الفعالة لـ CAD مجموعة من التدخلات الطبية وتغيير نمط الحياة. تعد المتابعة المنتظمة مع مقدمي الرعاية الصحية، إلى جانب التزام المريض بالعلاجات الموصوفة وتوصيات نمط الحياة، أمرًا محوريًا في تحسين النتائج وتحسين نوعية الحياة.
المضاعفات
1. سكتة قلبية
يمكن أن يؤدي انخفاض تدفق الدم المزمن أو الإصابة المتكررة لعضلة القلب بسبب النوبات القلبية إلى إضعاف القلب، مما يقلل من قدرته على ضخ الدم. تشمل أعراض قصور القلب التعب وضيق التنفس وتورم الساقين وانخفاض القدرة على ممارسة الرياضة. تركز الإدارة على تحسين هذه الأعراض وإبطاء تطور قصور القلب.
2. عدم انتظام ضربات القلب
يمكن لمناطق عضلة القلب المحرومة من تدفق الدم الكافي أو التي تعاني من ندوب من النوبات القلبية السابقة أن تعطل الإشارات الكهربائية الطبيعية للقلب، مما يؤدي إلى عدم انتظام ضربات القلب. يمكن أن تكون بعض عدم انتظام ضربات القلب حميدة ، في حين أن البعض الآخر يمكن أن يهدد الحياة ، ويتطلب تدخلات مثل الأدوية أو أجهزة تنظيم ضربات القلب أو مزيل الرجفان.
الموت القلبي المفاجئ:
3. الموت القلبي المفاجئ
يمكن أن تؤدي الانسدادات الشديدة أو الأضرار الكبيرة في عضلة القلب إلى عدم انتظام ضربات القلب القاتلة، مما يسبب الموت القلبي المفاجئ. إنها واحدة من أكثر المضاعفات الشديدة في CAD وتؤكد على أهمية الكشف المبكر وإدارة المرض.
4. سكتة دماغية
في حين أن مرض الشريان التاجي يؤثر على القلب، فإن نفس عملية تصلب الشرايين يمكن أن تؤثر على الشرايين في الدماغ. يمكن أن ينتقل تصلب الشرايين في الشرايين الدماغية، أو الجلطات المتكونة في القلب بسبب المضاعفات المرتبطة بأمراض الشريان التاجي، إلى الدماغ، مما يسبب السكتة الدماغية. تشمل أعراض السكتة الدماغية الخدر المفاجئ أو الضعف في الوجه أو الذراع أو الساق، خاصة على جانب واحد من الجسم، والارتباك، وصعوبة التحدث، وصعوبة المشي، والصداع الشديد. العناية الطبية الفورية أمر بالغ الأهمية.
وقاية
يعد منع مرض الشريان التاجي أمرًا محوريًا، ليس فقط للأشخاص المعرضين للخطر ولكن أيضًا لعامة السكان. يمكن تصنيف استراتيجيات الوقاية إلى تدابير أولية وثانوية:
1. عادات الأكل الصحية
- تناول نظامًا غذائيًا متوازنًا غنيًا بالخضروات والفواكه والحبوب الكاملة والبروتين الخالي من الدهون والدهون الصحية.
- الحد من تناول الدهون المشبعة والمتحولة والكوليسترول والصوديوم والسكريات المضافة.
- تحكم في أحجام الحصص للحفاظ على وزن صحي.
2. النشاط البدني المنتظم
- استهدف ممارسة التمارين الرياضية متوسطة الشدة لمدة 150 دقيقة على الأقل أسبوعيًا.
- قم بتضمين أنشطة تقوية العضلات لمدة يومين أو أكثر في الأسبوع.
3. الحفاظ على وزن صحي
- قم بحساب ومراقبة مؤشر كتلة الجسم (BMI) للبقاء ضمن نطاق صحي.
- ضبط السعرات الحرارية وممارسة الرياضة بانتظام لتحقيق والحفاظ على وزن صحي.
4. الإقلاع عن التدخين وتجنب التدخين السلبي
- اطلب المساعدة المهنية للإقلاع عن التدخين إذا لزم الأمر.
- تجنب التعرض للتدخين السلبي قدر الإمكان.
5. استهلاك الكحول المعتدل
- الحد من تناول الكحول بما يصل إلى مشروب واحد يوميًا للنساء ومشروبين يوميًا للرجال.
6. السيطرة على التوتر
- ممارسة تقنيات الحد من التوتر مثل اليقظة الذهنية أو التأمل أو اليوجا.
- الحرص على النوم والراحة الكافية.
7. الفحوصات الصحية المنتظمة
- مراقبة ضغط الدم ومستويات الكوليسترول والجلوكوز في الدم.
- استشر مقدمي الرعاية الصحية لإجراء فحوصات منتظمة ونصائح شخصية.
8. السيطرة على الظروف المزمنة
- إدارة حالات مثل مرض السكري وارتفاع ضغط الدم وارتفاع نسبة الكولسترول في الدم مع الأدوية على النحو الموصوف.
- قم بمراقبة هذه الحالات بانتظام حسب توجيهات مقدم الرعاية الصحية.
التكهن
يختلف تشخيص مرض CAD بناءً على عدة عوامل:
1. العوامل المؤثرة على التشخيص:
- شدة وموقع انسداد الشرايين.
- وجود حالات صحية أخرى مثل مرض السكري أو أمراض الكلى.
- التزام المريض بالعلاج وتوصيات نمط الحياة.
2. معدلات البقاء على قيد الحياة:
- ومع التقدم في العلاج، تحسنت معدلات البقاء على قيد الحياة لمرض الشريان التاجي على مر العقود.
- يلعب الاكتشاف والتدخل المبكر دورًا حاسمًا في تحسين النتائج.
3. نوعية الحياة بعد التشخيص:
- يمكن للعديد من المرضى أن يعيشوا حياة كاملة ونشطة مع الإدارة السليمة.
- يمكن لمجموعات إعادة تأهيل القلب والدعم أن تساعد المرضى على التكيف والحفاظ على نمط حياة صحي للقلب.
لا يزال مرض الشريان التاجي (CAD) يمثل مصدر قلق صحي كبير في جميع أنحاء العالم، حيث يؤثر على الملايين ويشكل تحديات في كل من التشخيص والإدارة. ومع ذلك ، مع التقدم في العلوم الطبية ، هناك الآن أدوات واستراتيجيات أكثر فعالية متاحة لاكتشافها المبكر والعلاج والوقاية منها. من خلال فهم تعقيدات مرض الشريان التاجي، بدءًا من الأعراض الأولية وحتى المضاعفات المحتملة، يمكن للأفراد اتخاذ قرارات مستنيرة بشأن صحة القلب. علاوة على ذلك ، فإن التركيز على تعديلات نمط الحياة ، مثل النظام الغذائي المتوازن ، وممارسة التمارين الرياضية ، والإقلاع عن التدخين ، يؤكد على قوة التدابير الوقائية. كما هو الحال مع العديد من الظروف الصحية ، فإن المعرفة والإدارة الاستباقية هي مفاتيح ضمان حياة أطول وأطول في مواجهة CAD.
علاجات العافية
امنح نفسك الوقت للاسترخاء
أقل الأسعار مضمونة!

أقل الأسعار مضمونة!
