
Spina Bifida: Types, Causes, and Symptoms
11 Oct, 2023
 Healthtrip Team
Healthtrip TeamSpina bifida is a congenital condition that occurs during early human fetal development when the neural tube fails to close properly, resulting in a gap in the spinal column. Ranging from subtle to severe forms, this defect can expose the spinal cord, impacting individuals across diverse populations. Recognizing the nuances of spina bifida is vital for timely intervention and ongoing care to enhance the quality of life for those affected.
Transform Your Beauty, Boost Your Confidence
Find the right cosmetic procedure for your needs.

We specialize in a wide range of cosmetic procedures

Types of Spina Bifida
1. Spina Bifida Occulta:
- Mildest form with a small gap in vertebrae.
- Often asymptomatic, may go unnoticed for years.
2. Meningocele:
- Protrusion of meninges through an opening.
- Spinal cord remains unexposed, visible sac-like protrusion.
3. Myelomeningocele:
- Most severe form with spinal cord protrusion.
- Neural elements exposed externally, high risk of complications.
Symptoms and Signs
A. Physical Symptoms
- Skin abnormalities over the spinal region (such as a dimple, birthmark, or abnormal hair growth).
- Visible spinal deformities or protrusions.
- Issues with bowel or bladder control.
- Orthopedic problems, including abnormal curvature of the spine (scoliosis) or joint contractures.
Most popular procedures in
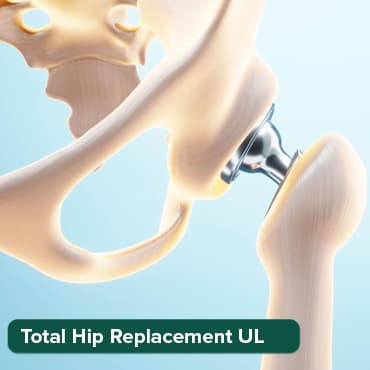
Total Hip Replacemen
Upto 80% off
90% Rated
Satisfactory
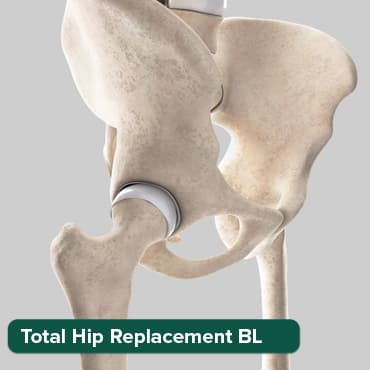
Total Hip Replacemen
Upto 80% off
90% Rated
Satisfactory
Breast Cancer Surger
Upto 80% off
90% Rated
Satisfactory

Total Knee Replaceme
Upto 80% off
90% Rated
Satisfactory
Total Knee Replaceme
Upto 80% off
90% Rated
Satisfactory

B. Neurological Symptoms
- Weakness or paralysis in the legs.
- Lack of sensation or numbness in the lower limbs.
- Difficulty with motor skills and coordination.
- Hydrocephalus (accumulation of cerebrospinal fluid in the brain), which may lead to an enlarged head.
C. Cognitive and Developmental Signs
- Learning disabilities.
- Challenges with memory and attention.
- Developmental delays, including delays in speech and language acquisition.
- Intellectual disabilities, varying in severity.
Causes
A. Genetic Factors
- Hereditary Influence: Increased risk if there is a family history of neural tube defects.
- Genetic Mutations: Certain genetic mutations may predispose individuals to spina bifida.
B. Environmental Factors
- Maternal Nutrition: Inadequate intake of folic acid during pregnancy.
- Exposure to Certain Substances: Certain medications or substances during pregnancy may contribute.
- Maternal Diabetes: Poorly controlled diabetes in the mother may increase the risk.
C. Folic Acid Deficiency
- Role of Folic Acid: Insufficient intake of folic acid during early pregnancy is a well-established risk factor.
- Neural Tube Development: Folic acid is crucial for the proper development of the neural tube in the fetus.
- Supplementation Importance: Adequate folic acid supplementation before and during pregnancy can significantly reduce the risk.
Diagnosis
A. Prenatal Diagnosis
- Ultrasound Imaging:
- Routine ultrasound examinations during pregnancy can identify spina bifida in some cases.
- Detailed imaging helps visualize the developing fetal spine and identify any abnormalities.
- Maternal Serum Alpha-Fetoprotein (MSAFP) Testing:
- Elevated levels of alpha-fetoprotein in maternal blood may indicate a neural tube defect, prompting further diagnostic testing.
- Amniocentesis:
- Collecting a sample of amniotic fluid allows for genetic analysis, aiding in the identification of chromosomal abnormalities and neural tube defects.
- Chorionic Villus Sampling (CVS):
- A sample of placental tissue is taken for genetic testing, providing insights into the fetal genetic makeup.
B. Postnatal Diagnosis
- Physical Examination:
- Visible spinal abnormalities and neurological signs are often apparent shortly after birth.
- The degree of severity is assessed through a physical examination of the newborn.
- Imaging Studies:
- Magnetic Resonance Imaging (MRI) and Computerized Tomography (CT) scans provide detailed images of the spinal cord and surrounding structures.
- Laboratory Tests:
- Genetic testing may be conducted to identify any associated genetic factors.
- Assessing alpha-fetoprotein levels in the infant's blood may be done to evaluate the extent of neural tube defects.
- Electrodiagnostic Tests:
- Electromyography (EMG) and nerve conduction studies may be performed to assess nerve function.
- Developmental Assessments:
- Ongoing developmental assessments are crucial to monitor cognitive and physical development over time.
Treatment
A. Surgical Interventions
- Closure of the Spinal Defect:
- For myelomeningocele, immediate surgical closure of the opening is typically performed to protect the exposed spinal cord.
- Surgical techniques aim to reduce the risk of infection and further damage.
- Orthopedic Surgeries:
- Corrective surgeries may be required to address orthopedic complications, such as scoliosis or joint deformities.
- Procedures aim to enhance mobility and minimize long-term musculoskeletal issues.
- Hydrocephalus Management:
- If hydrocephalus is present, surgical placement of a shunt may be necessary to divert excess cerebrospinal fluid away from the brain.
- Bladder and Bowel Procedures:
- Surgical interventions may be considered to address issues related to urinary and bowel control.
- Procedures aim to enhance functionality and quality of life.
B. Supportive Care
- Physical Therapy:
- Physical therapy is crucial for improving motor skills, strength, and coordination.
- Therapists work with individuals to enhance mobility and independence.
- Occupational Therapy:
- Occupational therapists assist individuals in developing daily living skills, enhancing independence in activities such as dressing, eating, and self-care.
- Speech and Language Therapy:
- For individuals with cognitive and communication challenges, speech and language therapy can be beneficial.
- Educational Support:
- Specialized educational programs and support services help individuals with spina bifida thrive academically.
- Psychological Support:
- Emotional and psychological support is vital for both individuals and their families.
- Counseling and support groups assist in coping with the challenges associated with spina bifida.
- Continued Medical Monitoring:
- Regular medical check-ups are essential to monitor the overall health of individuals with spina bifida.
- Ongoing assessments address emerging issues and guide adjustments to treatment plans.
Risk Factors
A. Family History
- Presence of spina bifida or other neural tube defects in close relatives increases the risk.
- Genetic factors may contribute to a familial predisposition.
B. Maternal Factors
- Maternal Age:
- Increased risk in pregnancies of women who are very young or advanced in age.
- Maternal Diabetes:
- Poorly controlled diabetes during pregnancy is associated with an elevated risk.
- Maternal Medication Use:
- Certain medications, especially anti-seizure drugs, may increase the risk.
Complications
A. Neurological Complications
- Paralysis:
- Depending on the location and severity of the spinal defect, paralysis of the lower limbs may occur.
- Hydrocephalus:
- Buildup of cerebrospinal fluid in the brain may lead to increased intracranial pressure.
- Neurogenic Bladder:
- Impaired bladder function due to nerve damage.
B. Orthopedic Complications
- Scoliosis:
- Abnormal curvature of the spine is a common complication.
- Joint Contractures:
- Limited range of motion and joint deformities may arise.
- Orthopedic Surgeries:
- Corrective surgeries may be needed to address musculoskeletal issues.
C. Cognitive Complications
- Learning Disabilities:
- Challenges in academic achievement and cognitive development.
- Intellectual Disabilities:
- Varying degrees of cognitive impairment may affect daily functioning.
- Speech and Language Delays:
- Communication difficulties may be present.
Prevention
A. Folic Acid Supplementation
- Preconception and Early Pregnancy:
- Adequate intake of folic acid before conception and during the early weeks of pregnancy is crucial.
- Reduces the risk of neural tube defects, including spina bifida.
B. Genetic Counseling
- Family Planning:
- Genetic counseling helps individuals with a family history of spina bifida make informed decisions about family planning.
- Assessing the risk and understanding preventive measures.
Wellness Treatment
Give yourself the time to relax
Lowest Prices Guaranteed!

Lowest Prices Guaranteed!





