
Arrhythmia: From detection to advanced treatment
08 Aug, 2023
 Healthtrip Team
Healthtrip TeamArrhythmia, often perceived as mere irregular heartbeats, delve deeper into the realm of cardiac health than many realize. These anomalies in our heart's rhythm can be subtle whispers of underlying conditions or loud alarms signaling immediate attention. As we navigate the intricate world of arrhythmias, understanding their origins, implications, and the advancements in their management becomes paramount. Join us on this journey to decode the mysteries of the heart's rhythm and its profound impact on our well-being.
Transform Your Beauty, Boost Your Confidence
Find the right cosmetic procedure for your needs.

We specialize in a wide range of cosmetic procedures

What is an arrhythmia?
An arrhythmia is any irregularity or abnormality in the heart's rhythm. It can be the heart beating too fast, too slow, or with an irregular pattern due to disruptions in the heart's electrical signaling.
The heart's electrical system controls the heartbeat's rate and rhythm. Proper electrical signaling ensures coordinated heart chamber contractions, allowing efficient blood flow. Disruptions can compromise the heart's ability to pump blood, leading to various symptoms and complications.
Anatomy and Physiology of the Heart
Four chambers of the heart
Most popular procedures in India
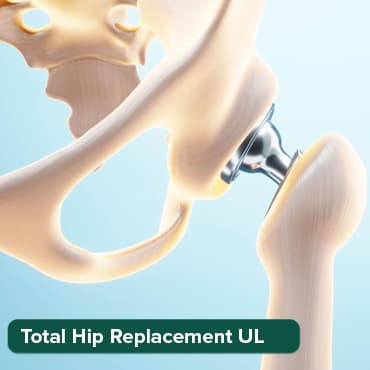
Total Hip Replacemen
Upto 80% off
90% Rated
Satisfactory
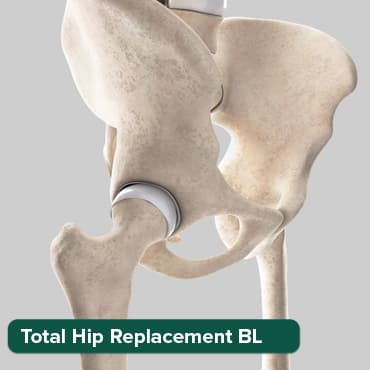
Total Hip Replacemen
Upto 80% off
90% Rated
Satisfactory
Total Hip Replacemen
Upto 80% off
90% Rated
Satisfactory

ANGIOGRAM
Upto 80% off
90% Rated
Satisfactory

ASD Closure
Upto 80% off
90% Rated
Satisfactory

The heart has four chambers: two atria (left and right) and two ventricles (left and right). Atria receive blood from the body and lungs, and ventricles pump blood out.
The cardiac conduction system
This system consists of specialized cells and pathways that generate and transmit electrical signals in the heart. These signals ensure a regular and coordinated heart rhythm.
- Sinoatrial (SA) node Located in the right atrium, the SA node is the heart's natural pacemaker. It initiates the electrical impulse, setting the heart's basic rhythm. The impulse causes the atria to contract and pump blood into the ventricles.
- Atrioventricular (AV) node Located between the atria and the ventricles, the AV node slows the electrical impulse before it reaches the ventricles. This delay ensures the atria contract and pump blood into the ventricles before they contract.
- Bundle of His This pathway transmits the electrical impulse from the AV node to the ventricles.
- Purkinje fibers:These fibers spread the electrical impulse throughout the ventricles, causing them to contract and pump blood to the body and lungs.
Classification of arrhythmia
1. Based on origin
- Atrial: These arrhythmias originate in the atria, the upper chambers of the heart. Common atrial arrhythmias include atrial fibrillation (AFib) and atrial flutter.
- Ventricular: These arrhythmias originate in the ventricles, the lower chambers of the heart. Examples include ventricular tachycardia (VT) and ventricular fibrillation (VFib).
- Bradycardia: This refers to a slower than normal heart rate, typically below 60 beats per minute in adults. Causes can include aging, heart damage, and certain medications.
- Tachycardia: This refers to a faster than normal heart rate, typically above 100 beats per minute in adults. It can originate in either the atria (atrial tachycardia) or the ventricles (ventricular tachycardia). Causes can range from fever and anemia to more serious conditions like high blood pressure or heart disease.
Common types of arrhythmia
1. Atrial Fibrillation (AFib)
- A rapid, irregular heartbeat that can lead to stroke and other heart-related complications.
- Causes: High blood pressure, coronary artery disease, chronic conditions like diabetes or asthma, and more.
- Symptoms: Palpitations, fatigue, dizziness, shortness of breath, and chest pain.
2. Atrial Flutter
- Similar to AFib but usually more organized and less chaotic rhythm than AFib. The heart's upper chambers (atria) beat too quickly, causing the heart to beat in a fast, regular rhythm.
- Causes: Often associated with other heart conditions like hypertension, heart disease, or hyperthyroidism.
- Symptoms: Palpitations, shortness of breath, and fatigue.
3. Supraventricular Tachycardia (SVT)
- An abnormally fast heartbeat originating above the heart's ventricles. It's not usually serious but can cause discomfort.
- Causes: Can be triggered by caffeine, nicotine, or alcohol. Other causes include certain medications, electrolyte imbalances, and some medical conditions.
- Symptoms: Rapid heartbeat, dizziness, chest pain, and shortness of breath.
4. Ventricular Tachycardia (VT)
- A fast, regular heartbeat that originates in the heart's lower chambers (ventricles). It can be life-threatening if not treated.
- Causes: Conditions that affect the heart, like cardiomyopathy, heart failure, or heart attack.
- Symptoms: Dizziness, fainting, palpitations, and shortness of breath.
5. Ventricular Fibrillation (VFib)
- A chaotic, rapid heartbeat that can lead to sudden cardiac arrest if not treated immediately.
- Causes: Heart attack, scarring of heart tissue from a prior heart attack, or certain medications.
- Symptoms: Loss of consciousness and no pulse.
6. Bradycardias:
- Sinus Bradycardia
- A slower than normal heart rate, typically below 60 beats per minute in adults.
- Causes: Aging, heart damage, medications, and conditions that can slow electrical impulses.
- Symptoms: Fatigue, dizziness, and lightheadedness.
7. Heart block
- A condition where the heart's electrical signal is delayed or blocked entirely as it moves from the atria to the ventricles.
- Causes: Aging, heart diseases, or as a side effect of certain medications.
- Symptoms: Fatigue, dizziness, and fainting
Causes of arrhythmia
1. Heart-related causes:
- Coronary artery disease: This is the narrowing or blockage of the coronary arteries due to plaque buildup, which can reduce blood flow to the heart muscle, potentially leading to arrhythmias.
- High blood pressure: Chronic high blood pressure can strain the heart and lead to thickening of its walls, which can disrupt the heart's electrical system.
- Heart failure: A condition where the heart doesn't pump blood as effectively as it should. The heart's weakened state can lead to arrhythmias.
- Heart surgery or procedures: Any surgery or procedure on the heart can potentially interfere with its electrical signals, leading to arrhythmias.
- Thyroid problems: Both hyperthyroidism (overactive thyroid) and hypothyroidism (underactive thyroid) can lead to arrhythmias.
- Certain medications and drugs: Some medications, both prescription and over-the-counter, as well as recreational drugs, can cause arrhythmias as a side effect.
- Excessive alcohol or caffeine consumption: Both substances can stimulate the heart and potentially lead to arrhythmias, especially when consumed in large amounts.
- Certain genetic conditions: Some people may inherit conditions that predispose them to arrhythmias. For instance, long QT syndrome is a genetic condition that can cause fast, chaotic heartbeats.
Symptoms of arrhythmia
- Palpitations: A sensation of skipped heartbeats, fluttering, or a racing heart.
- Dizziness or lightheadedness: Feeling unsteady or like you might pass out.
- Fainting (syncope): A temporary loss of consciousness, often described as "blacking out."
- Chest pain: Discomfort or pain in the chest, which can be sharp, dull, or squeezing in nature.
- Shortness of breath: Difficulty breathing or feeling like you can't get enough air.
Diagnosis of arrhythmias
Diagnosing arrhythmias—abnormal heart rhythms—typically involves a stepwise approach, including clinical evaluation, non-invasive tests, and possibly invasive testing. Here’s how arrhythmias are generally diagnosed:
a. Clinical Evaluation
- Symptom Review: Discussion of symptoms like palpitations, fainting (syncope), dizziness, chest pain, or shortness of breath.
- Medical History: Assessment of personal and family history of heart disease and risk factors for arrhythmias.
- Physical Exam: Checking for signs of heart disease, thyroid disease, or other conditions that could cause arrhythmias, such as a swollen thyroid gland or leg swelling.
b. Non-Invasive Diagnostic Tests
- Electrocardiogram (ECG or EKG): Records the electrical activity of the heart and can often identify the type of arrhythmia.
- Holter Monitor: A portable ECG device worn for a day or more to record heart activity over an extended period.
- Event Recorder: A device similar to a Holter monitor that records the heart's electrical activity when the patient activates it, typically used for intermittent symptoms.
- Echocardiogram: An ultrasound of the heart that can identify structural heart disease, problems with heart valves, or heart muscle function that may cause or contribute to arrhythmias.
- Stress Test: ECG monitoring during exercise to detect arrhythmias that are provoked by physical activity.
- Tilt Table Test: Used if syncope is a symptom, this test monitors heart rate and blood pressure responses to changes in position (lying to standing).
c. Advanced Non-Invasive Tests
- Cardiac MRI: Provides detailed images of the heart's structure and function, which can identify causes of arrhythmia.
- CT Scan: Can provide detailed images of the heart and detect potential structural causes for arrhythmias.
d. Blood Tests
To identify electrolyte imbalances, thyroid function, kidney function, and other potential causes of arrhythmias.
e. Invasive Diagnostic Tests
- Electrophysiological Study (EPS): A catheter-based test where wires are threaded into the heart to map electrical activity and induce arrhythmias under controlled conditions. This test can identify specific pathways of abnormal electrical conduction.
- Cardiac Catheterization: Although not typically used solely for diagnosing arrhythmias, this can identify coronary artery disease that might lead to arrhythmias.
f. Genetic Testing
May be considered if a hereditary condition is suspected, especially for conditions like long QT syndrome, Brugada syndrome, or hypertrophic cardiomyopathy.
g. Monitoring Implants
A small device implanted under the skin to continuously record the heart's electrical activity, often for up to three years, which is helpful for infrequent arrhythmias.
The specific diagnostic tools used will depend on the type of arrhythmia suspected and the patient's signs and symptoms. A cardiologist or an electrophysiologist—a cardiologist who specializes in heart rhythms—will usually oversee the diagnosis and treatment of arrhythmias.
Treatment and Management
1. Lifestyle changes:- Reducing or eliminating caffeine and alcohol intake.
- Quitting smoking.
- Managing stress through relaxation techniques like meditation or deep breathing exercises.
- Maintaining a healthy weight through diet and exercise.
- Regularly monitoring and managing blood pressure.
- Antiarrhythmics: Drugs that modify the electrical conduction system of the heart to restore a normal rhythm. Examples include amiodarone and flecainide.
- Beta-blockers: These reduce blood pressure and heart rate, helping to prevent some forms of arrhythmia. Examples include metoprolol and atenolol.
- Calcium channel blockers: These relax and widen blood vessels and slow the heart rate. Examples include diltiazem and verapamil.
- Anticoagulants: Also known as blood thinners, these reduce the risk of blood clots and stroke, which can be associated with some arrhythmias. Examples include warfarin and dabigatran.
- Cardioversion: A procedure where an electric shock is delivered to the heart to restore its normal rhythm. This can be done using electrodes placed on the chest or with a brief procedure.
- Ablation: Catheters are threaded through the blood vessels to the heart, and areas causing the arrhythmia are destroyed using radiofrequency energy.
- Pacemaker implantation: A small device is implanted under the skin near the collarbone. It sends electrical pulses to prompt the heart to beat at a normal rate.
- Implantable cardioverter-defibrillator (ICD): A device similar to a pacemaker but can deliver larger electric shocks to reset the heart rhythm when it detects dangerous arrhythmias.
- Maze procedure: Surgical creation of a series of precise incisions in the heart's atria to prevent the spread of erratic electrical signals.
- Coronary bypass surgery: This is primarily for coronary artery disease but can benefit some people with arrhythmias. It involves grafting vessels from elsewhere in the body to bypass clogged arteries, improving blood flow to the heart.
Complications of arrhythmia
- Stroke: Arrhythmias, especially conditions like atrial fibrillation, can lead to the formation of blood clots in the heart. If a clot breaks free, it can travel to the brain and block blood flow, causing a stroke.
- Heart failure: Chronic arrhythmias, especially if not properly managed, can weaken the heart and prevent it from pumping blood efficiently, leading to heart failure.
- Sudden cardiac arrest: Some severe arrhythmias, particularly ventricular fibrillation, can cause the heart to stop beating altogether. This is a medical emergency and can be fatal if not treated immediately.
Prevention of arrhythmia
- Engaging in regular physical activity.
- Avoiding smoking and excessive alcohol consumption.
- Managing stress through relaxation techniques.
- Medication adherence: For those prescribed medications for arrhythmias or other heart conditions, it's crucial to take them as directed to prevent complications.
- Avoiding triggers: For some people, caffeine, alcohol, certain medications, or even certain foods can trigger arrhythmias. Being aware of and avoiding personal triggers can help prevent episodes.
Recognizing and addressing arrhythmias at an early stage is crucial. Timely intervention can prevent complications, improve quality of life, and increase survival rates. Regular check-ups and being attuned to one's body, recognizing symptoms like unexplained dizziness, palpitations, or shortness of breath, can lead to early diagnosis and more effective management.
Advances in treatment and research: Over the years, significant strides have been made in understanding the mechanisms behind arrhythmias and in developing treatments. From sophisticated diagnostic tools to innovative surgical procedures and medications, the field continues to evolve. Ongoing research promises even more refined treatments in the future, emphasizing the importance of continued investment in cardiac research and patient education.
Wellness Treatment
Give yourself the time to relax
Lowest Prices Guaranteed!

Lowest Prices Guaranteed!







